“Never Event” Health Care Errors

Twenty years ago the Institute of Medicine (IOM) shocked the country with an expert estimate that as many as 98,000 people die in U.S. hospitals each year as a result of medical errors.1 By 2016, researchers from Johns Hopkins analyzed data from the CDC and estimated that this number had ballooned to as many as 250,000 deaths, making medical errors the third leading cause of U.S. mortality--behind only heart disease and cancer.2 The Institute for Health Care Improvement (IHI) likewise estimates that there are nearly 15 million instances of medical harm that occur each year in the United States, which translates to about 40-50 cases of patient harm for every 100 hospital admissions.3 These studies analyzed medical errors or harm broadly, recognizing they can occur from many different causes, and for numerous reasons. Sometimes, however, the medical error is so inexcusable or egregious that even the healthcare industry recognizes, fundamentally, it should have never occurred. We have all heard of or read about these types of cases of medical malpractice. They include bizarre situations like operations on the wrong patient or body part, surgical instruments left inside of patients, and drug overdoses that occur in a hospital. There are many never event errors that happen annually in U.S. healthcare facilities. It has been estimated that over 4,000 cases of never event surgical errors alone happen in the United States each year, with over 70% of them being fatal.4
What are "Never Events"?
In 2001, the CEO of the U.S. National Quality Forum (NQF) first called these inexcusable health care or medical errors "never events"--terms which are still used in the industry today.5 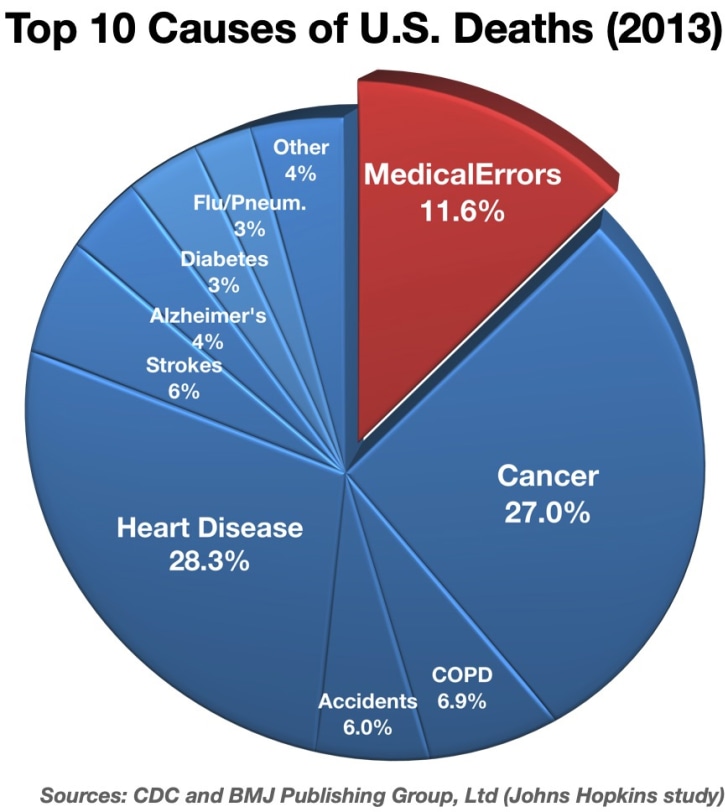 The NQF regards never events as "errors in medical care that are clearly identifiable, preventable, and serious in their consequences for patients, and that indicate a real problem in the safety and credibility of a health care facility."6 Since 2001, the list of health care never events has expanded, based on the fact that serious patient harm continues to occur in health care settings when it is typically preventable and where it should never occur. As of 2016, the same year of the Johns Hopkins medical error mortality study, the list of never events had reached almost 30 different situations.7
The NQF regards never events as "errors in medical care that are clearly identifiable, preventable, and serious in their consequences for patients, and that indicate a real problem in the safety and credibility of a health care facility."6 Since 2001, the list of health care never events has expanded, based on the fact that serious patient harm continues to occur in health care settings when it is typically preventable and where it should never occur. As of 2016, the same year of the Johns Hopkins medical error mortality study, the list of never events had reached almost 30 different situations.7
What are the Recognized Never Events?
There are 7 categories of health care events that should never happen, and there are several types within each category. The never events in each of these 7 categories are as follows:8
- Surgery and Procedure Never Events:
- on the wrong patient, body part, or with the wrong procedure
- foreign objects left inside patients (retained)
- death during or right after surgery in a normal, healthy patient.
- Medical Device or Product Related Never Events:
- contaminated devices or products
- devices or products used for different functions than they were intended
- devices/products that introduce air or gas bubbles into the patient's blood circulation, i.e. veins/arteries.
- Care Management Never Events – death or serious injury involving:
- medication errors (wrong patient, drug, drug preparation, drug route, drug overdose)
- unsafe administration of blood or blood products
- women in or following labor or delivery when they are low risk patients
- a newborn (neonate) related to labor or delivery
- a patient fall while being cared for in a healthcare facility
- stage 3 or 4 pressure ulcers that occur after admission to a healthcare facility
- lost biological specimens, including when it affects subsequent treatment decisions
- failure to follow up or communicate laboratory, pathology or radiology test results
- artificial insemination with the wrong donor sperm or egg.
- Radiology Never Events – death or serious injury related to metallic objects in the MRI area.
- Patient Protection Never Events:
- discharge of a patient or resident who is unable to make decisions, from a hospital, health care facility, or nursing home, to someone not authorized to take or transport them
- death or serious injury to a patient who is allowed to elope (disappearance)
- serious self-harm or suicide in a healthcare facility.
- Environmental Never Events -- death or serious injury due or related to:
- electric shock in a healthcare facility
- burns from any source in a healthcare facility
- bedrails or restraints in a healthcare facility.
- Criminal Never Events:
- Care ordered or given in a healthcare facility by someone impersonating or pretending to be a doctor, nurse, pharmacist, or another healthcare provider
- abduction of a patient or resident of any age
- physical or sexual abuse/assault of a patient or resident in or on the grounds of a healthcare facility.
How Common are Never Events?
It is difficult to know how many healthcare never events occur each year in the U.S. because hospitals and healthcare facilities are notorious for not always reporting them when they occur. This leads to health care never events being underreported annually in the U.S.9 Also, never events have legal (malpractice) and financial reimbursement ramifications. In fact, since 2008 Medicare has stopped reimbursing health care providers for many billions of dollars charged each year in connection with never events.10 And while Medicare provides statistics on "complications and deaths" in hospitals, the data does not disclose the number or percentage of never events by state or per health care institution.11
In South Carolina, most of this information is required to be reported by Medicare-Medicaid plans to the state's Department of Health and Human Services (SCDHH), although it is not easily accessible by the public.12 Additionally, only slightly more than half of U.S. states have enacted laws that mandate reporting (and tracking or corrective action) of serious, adverse, healthcare events; the rest of the states simply allow for "voluntary" reporting by health care facilities, which of course means that only a fraction of never events are actually reported.13
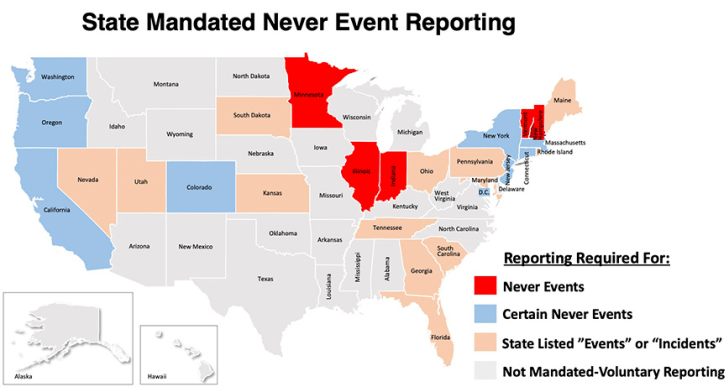
Further, although states that have mandatory reporting should have data for the vast majority of never events, even in these states the never events are still "grossly underreported,"14 and the reporting that does occur in most of these states does not separate out never events from other "incidents". This makes it difficult if not impossible for the general public to parse out never event statistics for health facilities. One of the reasons for this lack of publicly available data is that the health care industry fights against its disclosure.15 While there are websites that report hospital safety ratings/grades, including whether particular hospitals take steps to avoid harm or to manage never events, even then the online information usually does not reveal the numbers or types of never events statewide, or at specific healthcare institutions; and, many hospital or health care institutions decline to respond voluntarily or to provide any of this data.16 In South Carolina, hospitals are required to report "incidents resulting in death or serious injury" to the state Department of Health and Environmental Control (DHEC) Division of Health Licensing (DHL) within 10 days of the occurrence.17 Similar reporting requirements also exist in South Carolina for ambulatory surgical facilities, nursing homes, adult day care facilities, and other health care facilities.18 However, physicians themselves are exempt from these reporting requirements. In short, the information available to the public concerning never events is often difficult if not impossible to fully obtain. Yet, these inexcusable errors probably happen many, many thousands of times each year in the U.S..
What Should I Do if a Never Event Occurs?
Leapfrog, a non-profit patient safety organization for healthcare in the U.S., recommends that hospitals should take various steps when a never event occurs, such as apologizing to the patient/family, reporting the event, performing a root cause analysis and involving the patient/family in it, waiving costs of care associated with the event, and informing the patient/family of the actions the hospital will take to prevent a recurrence of the event, etc.19 Leapfrog also encourages the patient/family to talk with someone at the facility immediately about the event, including someone who can investigate, in a respectful yet assertive manner. This includes talking to the healthcare facility's customer service, patient advocacy and/or family relations department. They also suggest that the patient/family (or neutral person) communicating should be clear about expecting to hear back about the issue and that they should follow up. 20 Attorneys who handle medical malpractice cases also know it is vital for the patient/family to privately document the never event, including the names and job titles of health care providers who were involved and with whom they spoke about it. This should also include taking photos/video when possible. Further, you should talk with an attorney as soon as it is practical to do so, because the attorney may need to send letters to the healthcare providers/facility to preserve medical evidence, and to take other prudent legal steps.
The Lawyer's Role
A lawyer who is experienced in handling healthcare never event cases will know and understand these subjects and the pertinent medical statistics and information. He or she will be able to work with qualified expert witnesses in the field(s) of the particular never event(s) at issue, to determine how and why it occurred, and how it should have been prevented. Just because a hospital or healthcare facility apologizes for the never event, or agrees to waive part of a medical bill, does not mean that the healthcare provider will ever admit the never event was negligence, or that they will settle for a fair or reasonable amount. In fact, hospitals and other healthcare providers, and their defense attorneys, often dispute the claim or amount or deny that the never event amounted to neglect or caused serious harm, even after a lawsuit is filed.
Contact Us
The attorneys at Clore Law Group have significant experience and expertise with handling health care "never event" cases to a successful resolution. We have prosecuted many such cases and have obtained substantial settlements or jury awards for clients involving all of the following types of never events:
- foreign/retained objects left inside patients after surgery,
- death during or right after surgery in a normal, healthy patient,
- contaminated medical devices or products,
- medical devices or products used for different functions than they were intended,
- death or serious injury involving/due to:
- medication and drug errors (i.e. wrong patient, drug, drug preparation, drug route, drug overdose),
- unsafe administration of blood or blood products,
- women in or following labor or delivery when they are low risk patients,
- newborns (neonates) related to labor or delivery,
- patient falls while being cared for in a healthcare facility,
- stage 3 or 4 pressure ulcers that occur after admission to a healthcare facility,
- lost biological specimens, including when it affects subsequent treatment decisions,
- failure to follow up or communicate laboratory, pathology or radiology test results,
- failure to prevent patient elopement (disappearance),
- burns from a source in a healthcare facility, and
- physical or sexual abuse/assault of a patient or resident in or on the grounds of a healthcare facility.
If you or a loved one experienced a healthcare never event, you can email us at [email protected], or call us Toll-Free at 1-800-610-2546 for a free and confidential consultation.
Sources
- Kohn LT, Corrigan JM, et al, IOM Committee on Quality of Health Care in America, To Err is Human: Building a Safer Health System (Nat. Acad. Press 2000).
- Makary M, Daniel M, Medical Error‚ The third leading cause of death in the US, BMJ 2016; 353:i2139. Another recent study suggested an even higher number--as many 440,000 annual U.S. deaths due to medical errors, which is roughly 1/6 of all deaths in our country each year. See James JT, A New, Evidence-based Estimate of Patient Harms Associated with Hospital Care, J Patient Saf. Sep. 2013, Vol. 9, No. 3, pp. 122-28.
- Proctor L, IHI Launches National Campaign to Reduce Medical Harm, IHI Estimates That 15 Million Incidents of Patient Harm Occur in U.S. Hospitals Each Year, Feb. 2007, available online at: https://www.psqh.com/analysis/5-million-lives-ihi-launches-national-campaign-to-reduce-medical-harm/ See also National Quality Forum (NQF), Quality Connections, The Power of Safety: State Reporting Provides Lessons in Reducing Harm, Improving Care, June 2010, p. 1.
- Mehtsun WT, Ibrahim AM, et al, Surgical never events in the United States, Surgery 2016, Vol. 153, pp. 465-72 (2013).
- See https://www.leapfroggroup.org/never-events-report-2019.
- See the Centers for Medicare & Medicaid Services (CMS), Newsroom Fact Sheet, Eliminating Serious, Preventable, and Costly Medical Errors – Never Events, p. 1, May 18, 2006, citing the NQF: https://www.cms.gov/newsroom/fact-sheets/eliminating-serious-preventable-and-costly-medical-errors-never-events. The national hospital accrediting organization, the Joint Commission, uses "sentinel events," a broader category of health errors instead of never events. Sentinel events are patient safety events, i.e. unexpected occurrences not related to the patient's illness or condition, resulting in death, permanent harm, or severe temporary harm and intervention required to sustain life. https://www.jointcommission.org/resources/patient-safety-topics/sentinel-event/sentinel-event-policy-and-procedures/.
- PSNet, Never Events, fn.5.
- Id. See also the NQF, which also refers to never events as "serious reportable events" (SREs), although how many of these events are reported is widely disputed: http://www.qualityforum.org/Topics/SREs/List_of_SREs.aspx.
- See, e.g., Most Adverse Events at Hospitals Still Go Unreported, The Hospitalist, Vol. 7, July 2012, at: https://www.the-hospitalist.org/hospitalist/ article/125141/most-adverse-events-hospitals-still-go-unreported. See PSNet, Hospital Incident Reporting Systems Do Not Capture Most Patient Harm, Jan. 18, 2012, online at: https://psnet.ahrq.gov/issue/hospital-incident-reporting-systems-do-not-capture-most-patient-harm#, citing the U.S. Dep't of Health and Human Services Office of Inspector General Report of Jan. 2012, as well as the CMS Newsroom Fact Sheet, fn.8; and Farley DO, Haviland A, et al, Adverse-event-reporting practices by US hospitals: result of a national survey, quality & safety in healthcare, Vol. 17, 2008, pp. 416-23,
- See, e.g., Torrey T, Medicare's Never Events Policy, VeryWell Health, June 24, 2019, online at: https://www.verywellhealth.com/what-is-medicares-never-events-policy-2615384.
- See https://www.medicare.gov/hospitalcompare/Data/Data-Updated.html#%20 for information categories; and https://nashp.org/wp-content/uploads/2015/02/2014_Guide_to_State_Adverse_Event_Reporting_Systems.pdf.
- See the following South Carolina Dep't of Health & Human Services information online: https://msp.scdhhs.gov/SCDue2/sites/default/files/ Serious%20Reportable%20Events%20Guidance_032116_Final.pdf; https://www.scdhhs.gov/public-notice/provider-preventable-conditions. Also see the following: https://www.scdhhs.gov/internet/pdf/manuals-archive/Hospital/Section%202.pdf. Note, however, that Freedom of Information Act (FOIAA) requests can be made, https://www.scdhhs.gov/site-page/freedom-information-act-foia-request.
- See NQF Fact Sheet: Variability of State Reporting of Adverse Events, at: www.qualityforum.org. See also PSNet, (updated Sep. 2019)
- Kizer K, Stegun MB, Serious Reportable Adverse Events in Health Care, Advances in Patient Safety: From Research to Implementation, Vol. 4, p. 339 (2005).
- https://healthjournalism.org/blog/2011/04/cms-releases-hospital-by-hospital-data-on-never-events/("Hospitals continue to urge CMS not to publish these data,' read a March 31 [2011] joint statement from the AHA, the Federation of American Hospitals, and the Association of American Medical Colleges.").
- See also the Joint Commission: https://www.jointcommission.org/resources/ patient-safety-topics/sentinel-event/sentinel-event-data---general-information/.
- S.C. Code Regs § 61-16.702.
- Id. at § 61-91.600-601 (ambulatory surgical facilities); § 61-17.700-701 (nursing homes), § 61-75.700-703 (adult day care facilities).
- See Never Events, Patient Safety Network (PSNet), Sep. 2019 at https://psnet.ahrq.gov/primer/never-events
- Id.