Maternal Deaths are Increasing Due to Medical Malpractice

The rising incidence of maternal mortality in the United States has been referred to as a "national embarrassment."1 Compared to other wealthy nations, there are far too many American mothers who never get to hold their babies or watch them grow up, not to mention whose families and children who are devastated, as a result of medical malpractice. The tragic increase in the U.S. maternal death rate has occurred over the last 20 years even though we spend more on healthcare than any other country, and even though the maternal death rate has declined significantly in that time in other developed countries. Even worse, health care authorities point out that most of these mother's deaths in the U.S. are preventable.2
 What is Maternal Mortality?
What is Maternal Mortality?
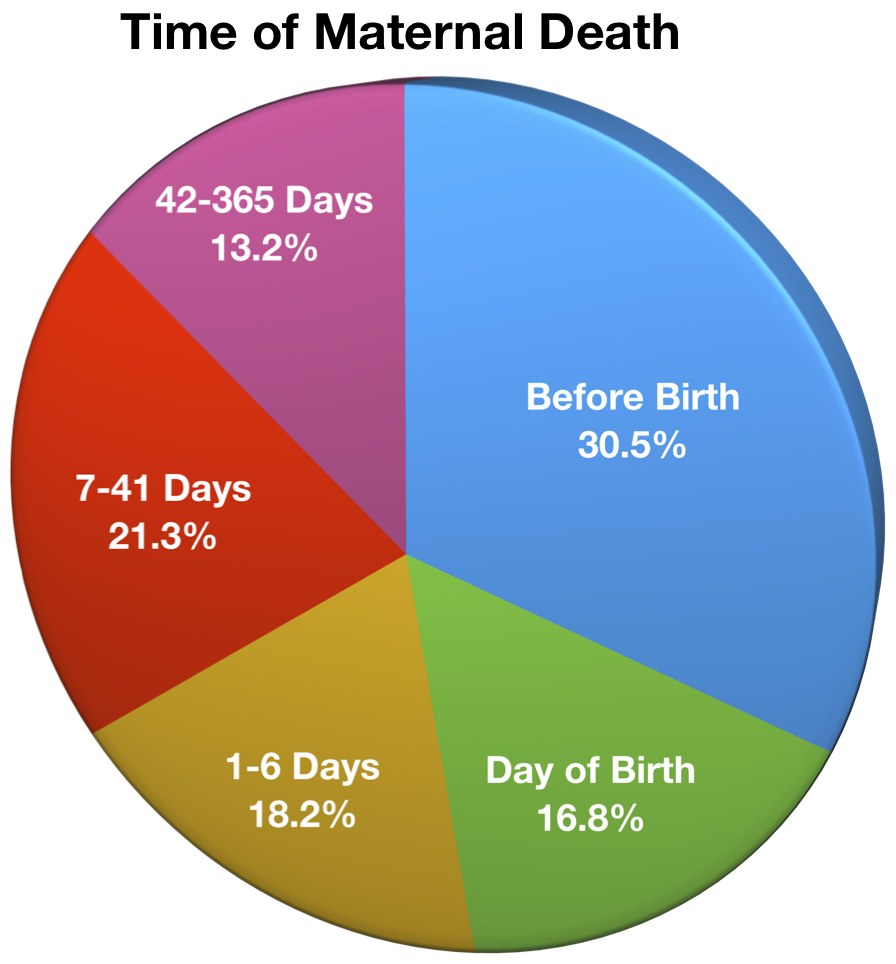
Maternal mortality is defined in the U.S to mean the death of a woman during pregnancy or up to one year after the end of a pregnancy, "from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes."3 Most of these pregnancy-related deaths occur during or up to 42 days from the end of pregnancy, which is the normal time period following pregnancy when a mother's physiologic changes revert back to normal.4 A pie chart illustrating the percentage breakdown in relation to the time of death before birth, on birth, or number of days after pregnancy is seen to the right.5
What are the Causes of Maternal Mortality?
While there are a number of causes of maternal death, and they vary by age and ethnicity among mothers, the most common categories, and percentages of time they have been reported to result in maternal death, are as follows6:
- Bleeding (14%) – hemorrhage, uterine rupture or atony, placental abruption, lacerations,
- Heart conditions (14%) – heart attack, aortic dissection, undiagnosed disorders, etc.
- Infection (10.7%) – including of the genital tract or following C-section, etc.
- Heart failure (10.7%) – cardiomyopathy, i.e. enlarged heart muscle in pregnancy.
- Blood clots (8.4%) – embolism into the lungs or brain, etc.
- Preeclampsia or eclampsia (7.4%) – from high blood pressure damage to organs/stroke, etc.
- Mental health conditions (7%).
Additionally, various other causes such as diabetes, high blood pressure, obesity, and age over 40 also put mothers at greater risk, thus resulting in complications that can lead to death.7
What is the U.S. Maternal Mortality Ratio?
The U.S. maternal mortality ratio is typically reported as the incidence of maternal death per 100,000 live births.8 Over a hundred years ago, in 1915, the maternal mortality ratio in the United States was 607.9 deaths per 100 live births.9 We made remarkable progress over the first three-quarters of the twentieth century with medical and technological advancements, resulting in a tremendous decrease in the incidence of maternal death. By 1987 the number of pregnancy-related deaths was just a fraction of that amount, we thought as low as 7.2/100,000 live births.10 As it turns out, we learned that there had been underreporting of these deaths in the 1980's and 1990's for many reasons, including different states using different coding in vital statistics records like death certificates, or using incompatible information about pregnancy status, cause and/or timing of death as compared to national norms.11 Over the past twenty-five years a concerted effort to track maternal mortality rates in the U.S. has occurred.12 We now know that maternal mortality has been rising over this time, and while it is much lower than a century ago, the ratio has roughly doubled or tripled in the latest quarter-of-a-century. This translates today into anywhere from 700—900 U.S. women who die each year from pregnancy-related conditions.13
What is the Trend Compared to Other Developed Countries?
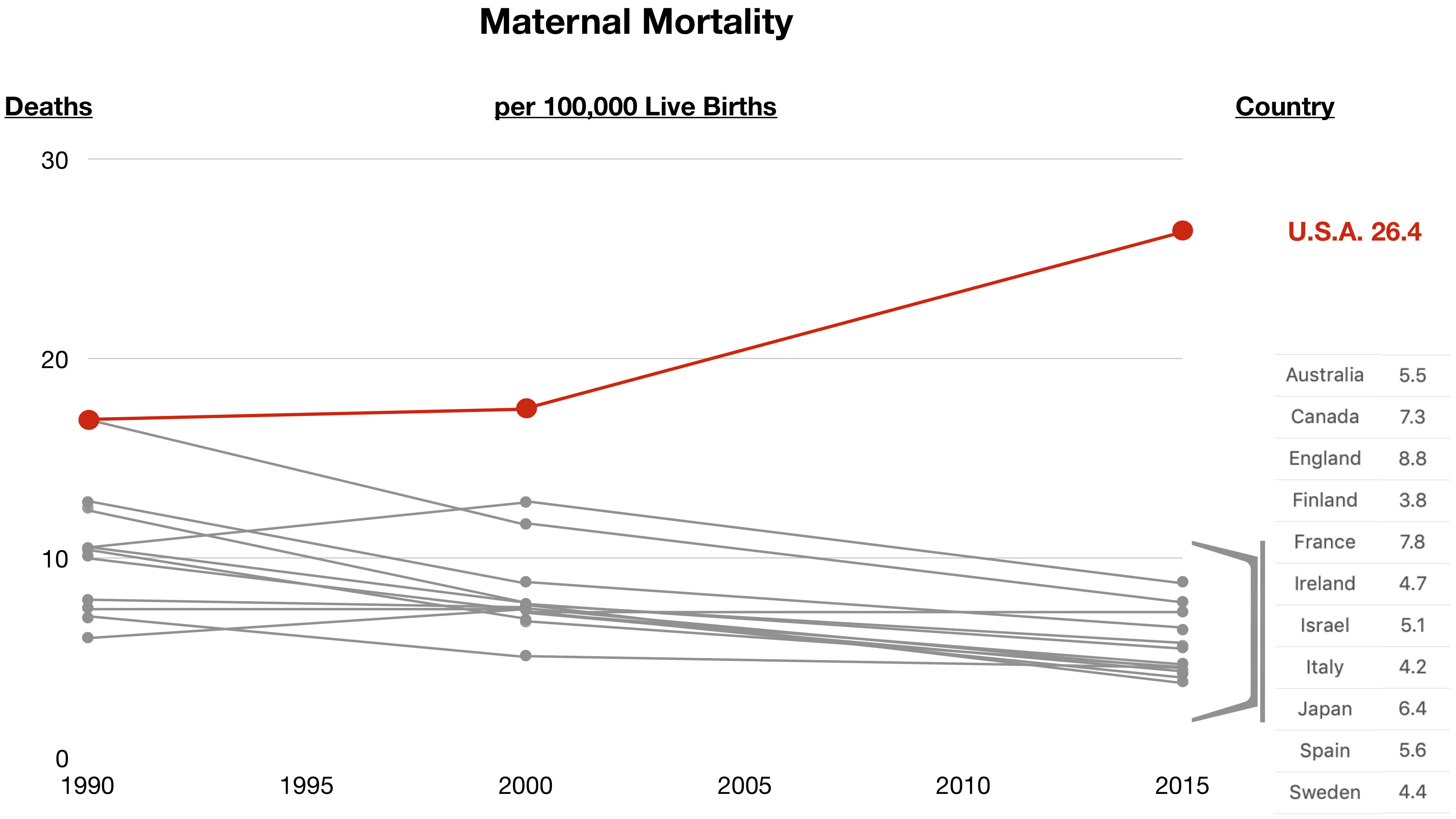
The World Health Organization (WHO) tracks maternal mortality for countries around the world. The WHO uses the same definition as that of the U.S. with the exception that their statistics are limited to deaths during pregnancy or within the first 42 days after pregnancy; the WHO uses another definition for later deaths that occur after 42 days but within a year of pregnancy. For international mortality comparison purposes, researchers and statisticians use the 42-day cut-off which has been a part of the U.S. National Vital Statistics System data since 2003.14 The shocking trend in the U.S. over the past 25 years can be seen in this graph that compares maternal mortality statistics from other developed countries for each of the years 1990, 2000, and 2015.15 Moreover, even by comparison to other less developed countries, the United States maternal mortality rate is substandard. For example, by 2015 the U.S. maternal mortality rate was higher than that in Iran, Libya and Turkey.16
What Kinds of Medical Malpractice Can Cause Maternal Death?
Recently, nine U.S. states17 joined in a project to delve deeper into medical and social records in cases of maternal mortality, to understand not only the causes of these deaths, and the effects of age and ethnicity, but also whether they could have been prevented. This involved considering what types of healthcare errors and factors led to maternal death. While obesity and chronic medical or other conditions made some patients at greater risk, the report revealed that the majority of time maternal death was preventable, but occurred due to health provider errors and factors such as medical malpractice involving the following conditions18:
- Bleeding (obstetrical hemorrhage)
- improper or inadequate assessment (estimation) of blood loss
- delays in diagnosis and ineffective treatment
- missed diagnosis
- lack of coordination of care
- improper or inadequate policies and procedures
- failure to educate patients on warning signs and need to seek care
- Heart conditions
- lack of knowledge
- delayed diagnosis and inappropriate treatment
- ineffective treatments
- lack of coordination of care
- inadequate or unavailable personnel
- failure to educate patients on warning signs and need to seek care
- Infection
- improper assessment
- delayed or missed diagnosis
- ineffective treatment
- lack of communication between healthcare providers
- inadequate training
- inadequate or unavailable personnel
- Heart failure (cardiomyopathy)
- Improper or inadequate assessment
- lack of knowledge and/or referral
- failure to screen
- ineffective treatment
- delayed or missed diagnosis
- failure to seek cardiologist (heart doctor) consultation
- Blood clots
- Lack of knowledge about the use of blood thinners and clot-busting drugs
- Preeclampsia or eclampsia
- delayed diagnosis or treatment
- use of ineffective treatments
- failure to seek consultation
- inadequate communication
- lack of communication as a barrier to coordination of healthcare
- Mental health conditions
- lack of communication between providers and patients/families
- lack of communication between providers
- inadequate outreach and support systems
- inadequate or unavailable personnel
How Do We Know that Healthcare Providers Can Do Better?
We know from the prior graph and data that the U.S. healthcare system should be able to reduce maternal mortality to a rate that is consistent with other developed countries, and certainly the level should not exceed that existing in Iran, Libya and Turkey. More importantly though, we already have a model in the United States, from California, of what type of action needs to be taken by all maternal health care providers in order to make this happen. In 2006, California's maternal mortality rate exceeded the national average. And so the state began a Maternal Quality Care Collaborative (CMQCC), initiated with Stanford University, to address the rising rate of maternal death and morbidity (injury). Since this time, "California has seen maternal mortality decline by 55 percent between 2006 and 2013, while the national maternal mortality rate continued to rise."19
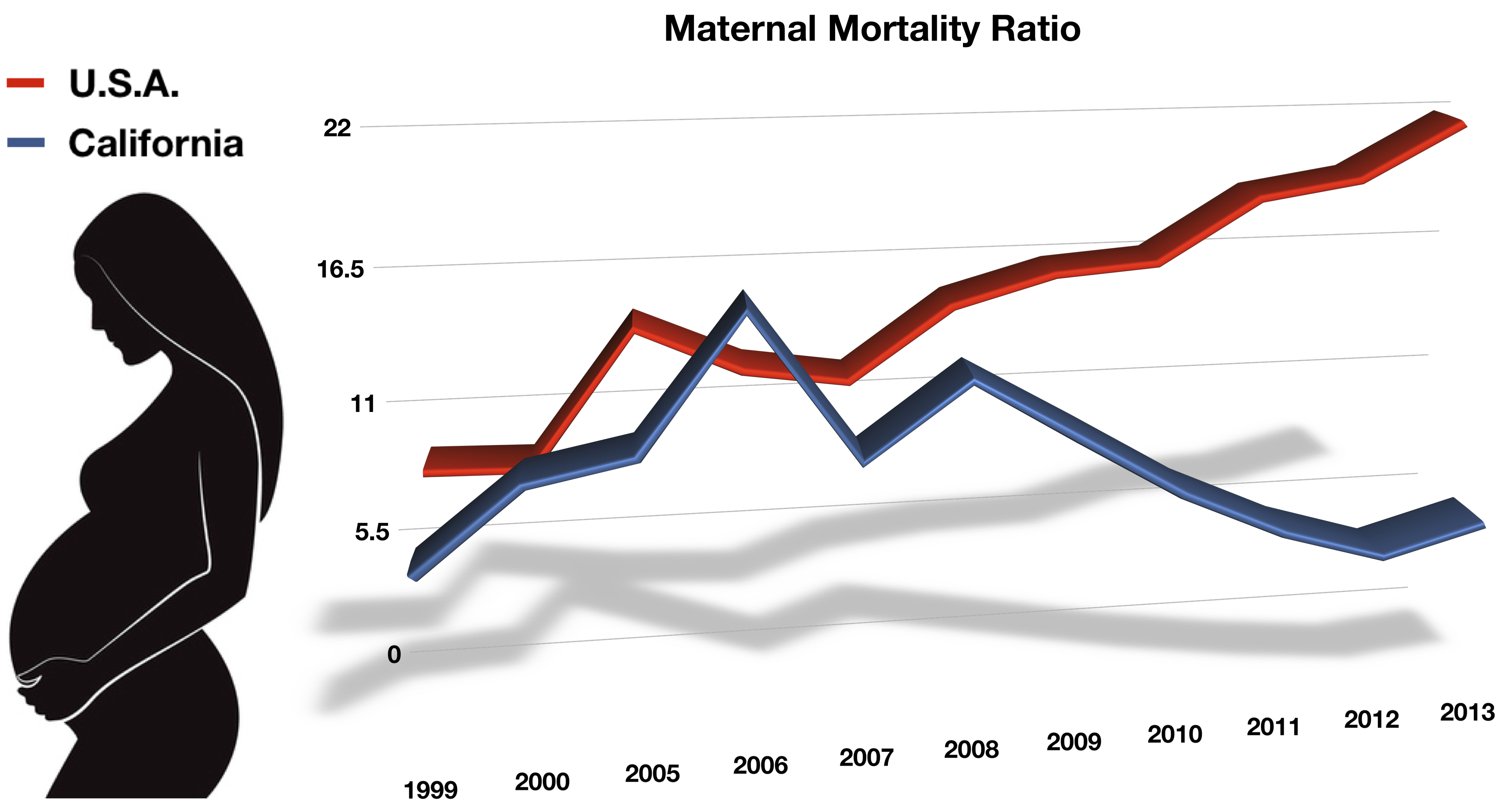
By comparing California's maternal mortality ratio over the last decade, we see a decline that resembles the maternal mortality ratio of other developed countries instead of the U.S. rate as a whole.20 The California initiatives that are responsible for a significant decline in maternal mortality and morbidity include greater healthcare provider education, training, toolkits, crash cart equipment, and numerous other matters designed to better diagnose, communicate, and treat patients with and following pregnancy-related conditions and disorders. Predictably, these initiatives focus on major categories of causes of maternal death21: (1) bleeding (obstetrical hemorrhage), (2) preeclampsia, (3) blood clots, and (4) heart disease and conditions. In short, the California initiatives are a model for reducing medical malpractice errors that result in maternal death.
The Lawyer's Role
The lawyer who is experienced in handling maternal mortality cases will know and understand the medicine and authoritative medical literature on the subject of pregnancy-related death. He or she will be able to work with qualified obstetricians, maternal-fetal medicine physicians, pathologists and other expert witnesses to determine how and why a mother died from a pregnancy-related condition, as well as if it was due to medical malpractice.
Contact Us
The attorneys at Clore Law Group have significant experience and expertise with handling maternal and pregnancy-related death cases to successful resolution. We have handled such medical malpractice cases where mothers have suffered death due to bleeding (hemorrhage) from conditions like placental abruption, genital tract lacerations from childbirth, and other conditions and causes. If a loved one or family member experienced death (or a severe injury such as brain injury) during or within a year from pregnancy due to any medical condition or healthcare that could possibly related to pregnancy or childbirth, you can email us at [email protected], or call us Toll-Free at 1-800-610-2546 for a free and confidential consultation.
Sources
- Ingraham C, Our maternal mortality rate is a national embarrassment (Wash. Post Nov. 18, 2015). See also Martin N, Propublica, Montagne R, U.S. Has the Worst Rate of Maternal Deaths in the Developed World (NPR May 12, 2017): https://www.npr.org/2017/05/12/528098789/u-s-has-the-worst-rate-of-maternal-deaths-in-the-developed-world.
- Id.; MacDorman ME, Declercq E, et al, Is the U.S. Maternal Mortality Rate Increasing? Disentangling trends from measurement issues, pp. 447-55 at 448, Obstet Gynecol. Vol. 128, No. 3 (Sep. 2016); Building U.S. Capacity to Review and Prevent Maternal Deaths, Report from Nine Maternal Mortality Review Committees, pp. 1-74, at 22 (2018)(estimating that overall "63.2% of pregnancy-related deaths were preventable").
- Center for Disease Control and Prevention (CDC), Pregnancy, Mortality Surveillance System: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-mortality-surveillance-system.htm, which is based on the International Classification of Diseases, Tenth Revision (ICD-10) for 1999. See Hoyert DL, Div of Vital Stat., Maternal Mortality and Related Concepts, Vital and Health Stat. Series 3, No. 33, pp. 1-14, at 3 (U.S. Dept of Health and Human Services, Public Health Service, National Center for Health Statistics Mar. 2007).
- Hoyert DL, Maternal Mortality and Related Concepts, n3, at 2.
- Adapted from Creanga AA, Syverson C, et al, Pregnancy-Related Mortality in the United States, 2011-2013, Vol. 130, No. 2, pp. 366-73 Obstet Gynecol. (Aug. 2017).
- Id. at 8-10; Report from Nine Maternal Mortality Review Committees, n2, at 14, 21, 26-28.
- See, e.g., https://www.americashealthrankings.org/explore/health-of-women-and-children/measure/ maternal_mortality.
- Center for Disease Control and Prevention (CDC), Pregnancy, Mortality Surveillance System, n3, at 1.
- Hoyert DL, Div of Vital Stat., Maternal Mortality and Related Concepts, n3, at 2.
- Id.; Center for Disease Control and Prevention (CDC), Pregnancy, Mortality Surveillance System, n3, at 2; MacDorman ME, Declercq E, et al, Is the U.S. Maternal Mortality Rate Increasing? Disentangling trends from measurement issues disentanglement, n2, at 2-12.
- MacDorman ME, Declercq E, et al, Is the U.S. Maternal Mortality Rate Increasing? Disentangling trends from measurement issues, n2, at 2-4.
- Id.; Hoyert DL, Div of Vital Stat., Maternal Mortality and Related Concepts, n3; Wetzel LM, Maternal Mortality Statistics, Contemp OB/Gyn (Jan 11, 2018)(noting at p. 3 the 2 sources of maternal mortality data in the U.S. today stem from the National Center for Health Statistics (NCHS) and the Pregnancy Mortality Surveillance System (PMSS-MM)).
- Building U.S. Capacity to Review and Prevent Maternal Deaths, Report from Nine Maternal Mortality Review Committees, n2, at 6; Fields R, Sexton J, How Many American Women Die From Causes Related to Pregnancy or Childbirth? No one Knows, ProPublica (Oct. 23, 2017).
- MacDorman ME, Declercq E, et al, Is the U.S. Maternal Mortality Rate Increasing? Disentangling trends from measurement issues, n2, at 2-4 (noting that a number of states have been slow to adopt this criterion over the decade since, and these difficulties have been part of the reason that the U.S. has not formally published an official mortality rate since 2007, which the author characterizes as an "international embarrassment."). See also Fields R, Sexton J, How Many American Women Die From Causes Related to Pregnancy or Childbirth?, n13.
- Adapted from GBD 2015 Global Maternal Mortality Collaborators, Global, regional, and national levels of maternal mortality, 1999-2015: a systematic analysis for the Global Burden of Disease Study 2015, The Lancet Vol. 388, pp. 1775-812 (Oct. 8, 2016). Note that the only years of comparison given in the study were for 1990, 2000, and 2015.
- Id. at 1789-90.
- Building U.S. Capacity to Review and Prevent Maternal Deaths, Report from Nine Maternal Mortality Review Committees, n2, at 6-10 (the nine states are Colorado, Delaware, Georgia, Hawaii, Illinois, North Carolina, Ohio, South Carolina, and Utah).
- Id. at 24-28.
- CMQCC website, accessed on 12/9/18 at: https://www.cmqcc.org/who-we-are.
- Id.
- Id. at https://www.cmqcc.org/qi-initiatives, accessed on 12/19/18.