Surgical Errors and “Never Events”

We all know that when we sign a consent form to undergo an operation, things can go wrong in the surgery. But this does not mean that we have consented to improper, substandard, or negligent care amounting to medical malpractice, and especially not to grossly improper care.
Surgical and anesthesia consent forms are required by law to allow the health care professionals to legally perform surgery, and to legally provide anesthesia and care for us in an operation or procedure. The signed consent form documents our agreement beforehand, so that the surgery does not amount to a legal assault or battery, i.e. criminal act, on us. Surgical errors that occur because of wrongdoing are not part of a consent form, however, and instead they can be the basis of a civil action or lawsuit to recover money damages for the harm caused by this medical malpractice.
What are Surgery Never Events?
Surgery "never events" are errors that occur in or right after surgery that cause patient harm and that should never happen.1 It has been estimated that over 4,000 cases of never event surgical errors happen in the United States each year, with over 70% of them being fatal.2 These shocking events involve 3 different categories of errors: (1) surgery involving the wrong patient, body site, side, or surgery; (2) retained surgical (foreign) objects—i.e. objects left inside a patient after surgery that should have been removed; and, (3) death during or right after surgery in a normal, healthy patient.3
1. Wrong Patient, Site, Side, or Surgery
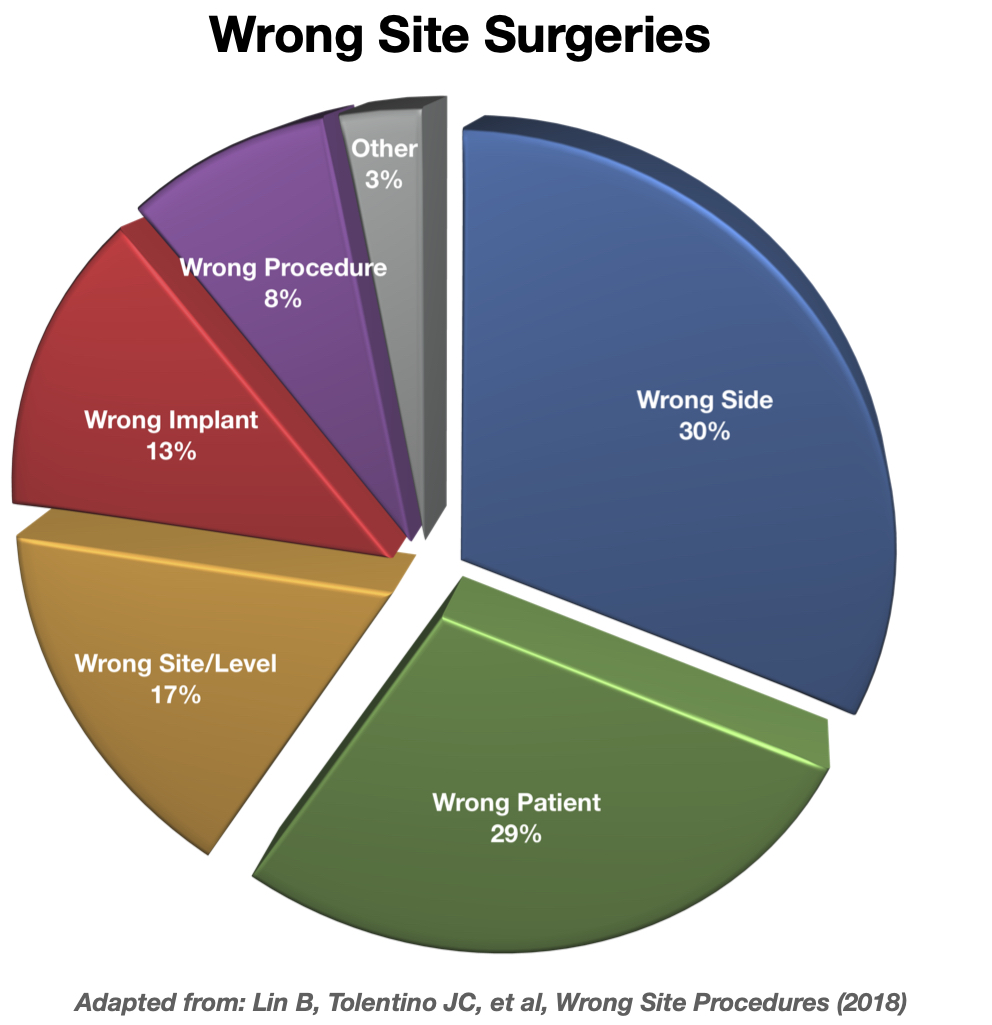
Even though it is almost unfathomable how these things can happen, surgeries that are performed on the wrong patient, site/side of the body, or with the wrong implant or procedure continue to happen far too often. These situations have specific meanings4:
- Wrong patient: means there was an incorrect identification of the patient, so that the surgery or procedure occurred on the unintended patient.
- Wrong surgery: means the surgery performed was not the one intended and is inconsistent with the signed consent form.5 But it can also include unnecessary surgery.6
- Wrong site: can mean that a procedure occurred to the wrong area or location of the body, or "catch all" terms for the wrong patient, side, level/part, and/or procedure/surgery.
- Wrong side: means an invasive procedure occurred on the incorrect side of the body.
- Wrong level/part: means the surgery occurred at the correct site or part of the body (example: lumbar spine) but at the wrong level or part of that site (ex.: L2 instead of L3).
- Wrong implant: means the prosthesis or device implanted was other than what was intended for the procedure or surgery.
A percentage breakdown of these types of surgical errors has been reported from various studies seen in the pie-chart below7:
All of these wrong site surgeries can and should be prevented. The Joint Commission on hospital accreditation and other organizations have had universal protocol since 2003 to eliminate these never events, and hospitals and surgical staff should follow them. This 3-step protocol involves: (1) a preoperative verification process, (2) clearly marking the correct surgical site/structures, and (3) taking a "time out" immediately before the procedure begins.8 Yet, these types of surgical errors continue to occur due to many factors, including:
- Inadequate assessment of the patient, review of preop/medical records, or planning
- Failure to include the patient and family to identify the surgical site
- Failure to clearly mark or identify the surgical site
- Miscommunications or incomplete communications among surgical team members
- Failure to recheck the patient before the procedure begins
- Lack of institutional protocol to verify the correct surgical site
- Lack of use of checklists or proper supervision
- Unusual time pressures, stress, or fatigue prior to or during surgery
- Change of surgical team members such as nursing personne
- Lack of availability of information or personnel
- Inadequate orientation and training of personnel.9
2. Retained Surgical Bodies (Foreign Objects)
Some foreign objects are of course meant to be left in a patient's body after surgery—i.e. orthopedic implants, prosthetics, pacemakers, etc. But when an object used for surgery is not intended to be, nor should it be, left inside the patient after surgery, then another fundamental error has occurred. This includes the following type of surgical equipment10: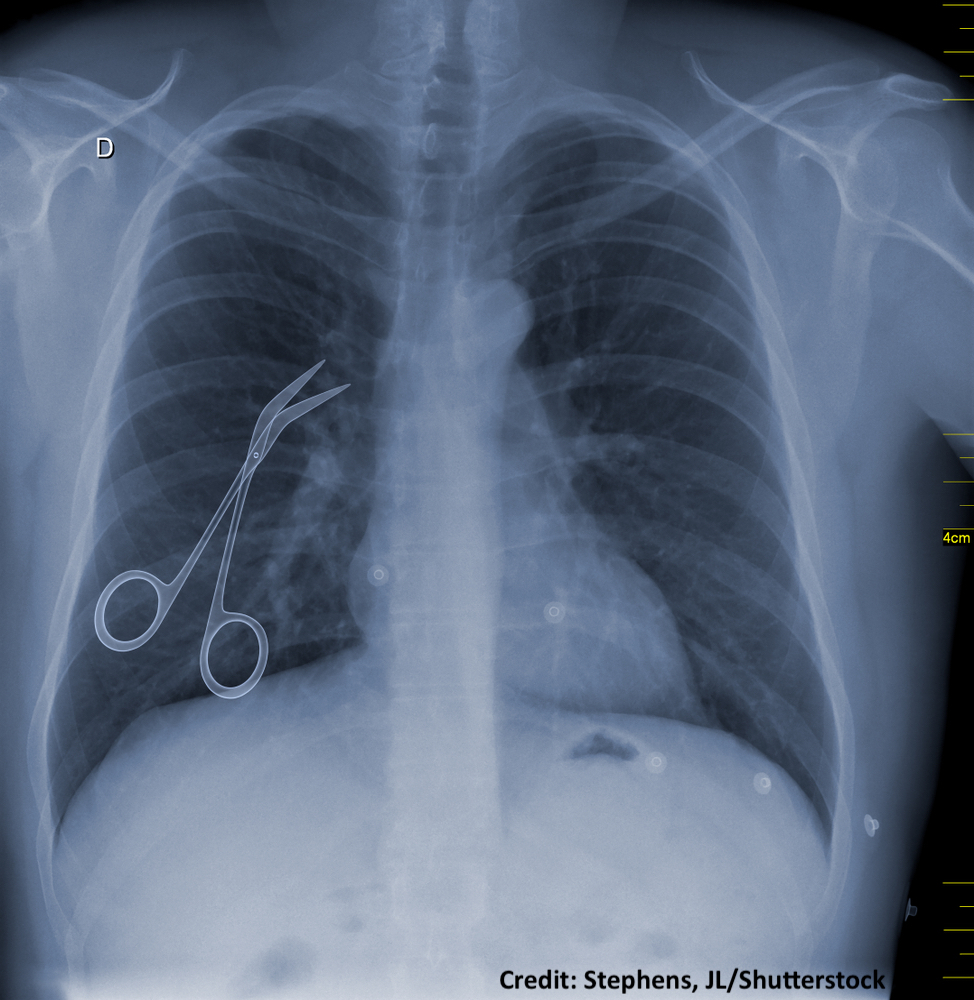
- Sponges
- Clamps
- Retractors
- Needles
- Trocars
- Scissors
- Scalpels
- Electrodes
- Drains
An important part of an operation is known as the surgical or instrument "count." This is where equipment used in surgery is counted—meaning sponges (and swabs, compresses, dressings, towels, etc.), sharps (needles, scalpels, pins, electrocautery tips, saw blades, drills, etc.) and instruments (clamps, retractors, scissors, electrodes, drains, and other parts such as suction tips, wing nuts, blades, sheathes, etc.). The surgical counts occur at multiple steps, including before the incision and at closing the surgical site/wound/skin. These counts are the responsibility of the perioperative nurses (circulating nurse, scrub nurse/tech), and should occur in an audible, systematic and methodical fashion, which is normally part of facility protocol, policies and/or procedures. Surgical counts are documented on the intraoperative/nursing record, and if there is a discrepancy (between what went in the patient and what came out or is missing), then a recount is typically conducted. If there is still an object missing, then the count discrepancy is reported to the surgeon. At this point there should be a manual inspection of the operative site and a visual inspection of the area around the surgical field, e.g. floor, buckets, linen and trash receptacles, etc. If possible, surgery is suspended until the missing item(s) is/are located. Intraoperative X-rays are also normally taken to ensure the missing object(s) were not inadvertently left inside the patient.11
So, there are multiple steps that should be taken during surgery to prevent surgical objects from being left inside of patients. Invariably, healthcare human error at one these steps is what leads to a surgical object being retained in the patient's body. This can happen for various reasons, such as if the "count" is mistakenly reported as correct when it is not (failure to properly count, miscounting, math error, etc.), or when a missing object is identified in the count but inappropriate steps are taken to locate it (no detailed searching, no X-rays, inadequate X-rays, misreading of X-rays, etc.). When this happens, patients may thereafter develop significant pain, infection, problems with healing (fistulas), scarring (adhesions) inside their bodies, obstructions, bowel perforation, and even death. And obviously a second surgery is required to remove the foreign object(s) if possible.12
3. Death During or Right After Surgery in a Normal, Healthy Patient

Surgical risk of death depends significantly on the type of procedure, the nature of it (elective, urgent or emergent), patient age, and the patient's preexisting conditions. But surgical and anesthesia skill and the quality of care is also very important.13 Hospital consent forms always list risks like surgical bleeding (hemorrhage), infection, and death. When an otherwise normal, healthy patient14 undergoes an elective or non-emergent procedure and dies during or right after that procedure, a serious healthcare error has almost always occurred.
Usually, death during or soon after surgery in these patients is either from blood loss because of severe internal/arterial bleeding that was caused and/or not controlled by the surgeon when it should have been, or because of anesthesia that was not properly monitored or corrected by the anesthesia provider (anesthesiologist or CRNA)—leading to breathing failure from the airway or lungs. Yet sometimes death can be due: to wrong site surgeries;15 surgical damage (puncture, laceration, penetration, etc.) to an organ;16 early removal of the breathing tube;17 heart failure, stroke or brain damage/paralysis from very low blood pressure,18 or other causes.
"Never events" that occur in surgery have also been reported or alleged to cause death in the days or weeks after surgery, including from situations like blood transfusion errors in surgery that result in shock which is ultimately fatal,19 or from contaminated surgical instruments resulting in severe infection (sepsis) and death.20
Is a Lawsuit Necessary?
Just because surgical errors should never happen does not mean that a surgeon, healthcare institution or provider will ever admit that it occurred due to their negligence or malpractice, or that they will settle with the victim for a fair or reasonable amount. In fact, surgeons, healthcare facilities, providers, and their attorneys often deny wrongdoing and responsibility in court, and claim that the error did not amount to negligence and/or did not cause any serious or permanent injury. As a result, civil lawsuits for medical malpractice (negligence) are typically the only way to seek accountability and justice.
Contact Us
The lawyer who is experienced in handling surgical and surgery error cases will know and understand these subjects and the important aspects of the surgery and medical information. He or she will be able to work with qualified expert witnesses in the field(s) of surgery, nursing, anesthesiology, and other fields to determine and prove how and why it occurred, and how it should have been prevented. The attorneys at Clore Law Group have significant experience and expertise with handling surgical and surgery error cases to successful resolution. We have successfully prosecuted surgical error “never event” cases such as retained surgical bodies involving foreign instruments (sponges, needles), and cases of death during or soon after surgery, as well as a number of other cases involving medical malpractice that occurred in surgery.
If you or a loved one experienced a surgical error and harm, you can email us at [email protected], or call us Toll-Free at 1-800-610-2546 for a free and confidential consultation.
Sources
- See Never Events, Patient Safety Network (PSNet), Sep. 2019 at https://psnet.ahrq.gov/primer/never-events. See also the Centers for Medicare & Medicaid Services (CMS), Newsroom Fact Sheet, Eliminating Serious, Preventable, and Costly Medical Errors – Never Events, p. 1, May 18, 2006, citing the NQF, available at: https://www.cms.gov/newsroom/fact-sheets/eliminating-serious-preventable-and-costly-medical-errors-never-events.
- Mehtsun WT, Ibrahim AM, et al, Surgical never events in the United States, Surgery 2016, Vol. 153, pp. 465-72 (2013).
- See Never Events, Patient Safety Network (PSNet), Sep. 2019 at https://psnet.ahrq.gov/primer/never-events. See also the National Quality Forum (NQF), which also refers to never events as “serious reportable events” (SREs), http://www.qualityforum.org/Topics/SREs/List_of_SREs.aspx. See the following articles for a discussion of underreporting that occurs by healthcare institutions and providers with respect to serious reportable events: Most Adverse Events at Hospitals Still Go Unreported, The Hospitalist, Vol. 7, July 2012, at: https://www.the-hospitalist.org/hospitalist/article/125141/most-adverse-events-hospitals-still-go-unreported. See PSNet, Hospital Incident Reporting Systems Do Not Capture Most Patient Harm, Jan. 18, 2012, online at: https://psnet.ahrq.gov/issue/hospital-incident-reporting-systems-do-not-capture-most-patient-harm#, citing the U.S. Dep’t of Health and Human Services Office of Inspector General Report of Jan. 2012, as well as the CMS Newsroom Fact Sheet, fn.8; and Farley DO, Haviland A, et al, Adverse-event-reporting practices by US hospitals: result of a national survey, quality & safety in healthcare, Vol. 17, 2008, pp. 416-23,
- Lin A, Wernick B, et al, Wrong-Site Procedures: Preventable Never Events that Continue to Happen - Vignettes in Patient Safety, Vol. 2, Firstenberg MS, Stawicki SP, Intech Open (Jan. 10, 2018), p. 4/15, available online at: https://www.intechopen.com/books/vignettes-in-patient-safety-volume-2/wrong-site-procedures-preventable-never-events-that-continue-to-happen.
- See the Centers for Medicare and Medicaid Services (CMS) Decision Memo: Wrong Surgery Performed on a Patient (CG-00401N)
NCAId=221&ver=17&NcaName=Surgery+on+the+Wrong+Patient&bc=BEAAAAAAEAAA&&fromdb=true, where CMS points out that charges associated with the “wrong surgery” are not reimbursable, which is also the case for “wrong patient” surgeries, https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=221&ver=17&NcaName=Surgery+on+the+Wrong+Patient&bc=BEAAAAAAEAAA&&fromdb=true, surgeries on the “wrong body part, and other never events.
- See, e.g., Kealey B, A “Never Event” Happened to My Family Member. Don’t Let it Happen to You, Society of Hospital Medicine (SHM), The Hospital Leader, Dec. 8, 2015, at: https://thehospitalleader.org/a-never-event-happened-to-my-family-member-dont-let-it-happen-to-you/.
- See, e.g., Lin, Wrong-Site Procedures, fn.4, above.
- Joint Commission, Universal protocol for preventing wrong site, wrong procedure, wrong person surgery (2003), at: https://www.jointcommission.org/standards/universal-protocol/.
- Id. See also Patient Safety and Quality: An Evidenced-Based Handbook for Nurses, Ch. 36, Mulloy DF, Hughes RG, Wrong-Site Surgery: A Preventable Medical Error, 2-381-2-395, at: https://www.ncbi.nlm.nih.gov/books/NBK2678/; White J, Avoid ‘Never Events’ in Surgery: 4 Areas to Watch, Jul. 11, 2015, available online at: http://www.healthcarebusinesstech.com/avoid-never-events-surgery/; Gawande AA, Studdert DM, Patient Safety: Risk Factors for Retained Instruments and Sponges after Surgery, NEJM Vol. 348, pp. 229-235 (2003); PSNet, Wrong-Site, Wrong-Procedure, and Wrong Patient Surgery, Sep. 2019, at: https://psnet.ahrq.gov/primer/wrong-site-wrong-procedure-and-wrong-patient-surgery; and Health Research & Educational Trust and Joint Commission Center for Transforming Healthcare, Reducing the risks of wrong-site surgery: Safety practices from The Joint Commission Center for Transforming Healthcare project, accessible at: https://www.aha.org/system/files/2018-01/reducing-risks-wrong-site-surgery-safety-practices-joint-commission-center-transforming-healthcare-project-2014.pdf.
- See, e.g., Nguyen MC, Moffatt-Bruce SD, What’s New in Academic Medicine? Retained Surgical Items: Is “zero incidence” achievable? Vol. 2, Int J Acad Med. pp. 1-4 (2016)
- See the World Health Organization (WHO), Patient Safety, WHO Guidelines for Safe Surgery 2009, Objective 7: The team will prevent inadvertent retention of instruments and sponges in surgical wounds, pp. 72-74. See also the Association of periOperative Registered Nurses (AORN), Recommended Practices for Sponge, Sharp and Instrument Counts is Up for Review, Apr. 1, 2005, in Infection Control Today, available online at: https://www.infectioncontroltoday.com/guidelines/aorns-recommended-practices-sponge-sharp-and-instrument-counts-review; the Association of Surgical Technologists (AST), Recommended Standard of Practice for Counts, at: https://www.ast.org/uploadedFiles/Main_Site/Content/About_Us/Standard%20Counts.pdf, and Gibbs VC, NoThing Left Behind®: the Prevention of Retained Surgical Items Multi-stakeholder Policy – Job-Aid Reference Manual, at: http://www.nothingleftbehind.org/uploads/NoThing_Left_Behind_PRSI_Policy_2018.pdf.
- Id.; Gawande, Risk Factors for Retained Instruments and Sponges after Surgery, fn.8 above. See also Nguyen, Retained Surgical Items, fn.8 above; and Gibbs, NoThing Left Behind®, fn.10 above.
- See, e.g., Whitlock J, The Risk of Death from Surgery, Verywell Health, Dec. 10, 2019, at: https://www.verywellhealth.com/what-is-the-risk-of-death-from-surgery-3157294.
- These never events refer to normal, healthy patients as defined by the American Society of Anesthesia (ASA) Class I patient, i.e. patients such as those who are healthy, non-smokers, and have minimal or no alcohol use. See: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system.
- See, e.g., Mehtsun, Surgical never events in the United States, fn.2 above.
- See, e.g., Kwiatt M, Tarbox A, et al, Thoracostomy tubes: A comprehensive review of complications and related topics, Vol. 4, No. 2, Int J Crit Illn Sci., pp. 143-55 (Apr-Jun 2014), available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4093965/?report=printable, and MDedge/OBGyn, Medical Verdicts, Bowel perforation causes woman’s death: $1.5M verdict, Vol. 25, No. 8, OBG Manag., pp.47-48 (Aug. 2013), at: https://www.mdedge.com/obgyn/article/76833/practice-management/bowel-perforation-causes-womans-death-15m-verdict.
- See, e.g., Kita J, Doctors Confess Their Fatal Mistakes, Aug. 20, 2019, TheHealthy, accessible online at: https://www.thehealthy.com/healthcare/doctors/doctors-confess-their-fatal-mistakes/.
- See, e.g., Cullen DJ, Kirby RR, Beach Chair Position May Decrease Cerebral Perfusion, Anesthes Patient Saf Found. (APSF) Newsletter, Vol. 22, No. 2 (Summer 2007), online at: https://www.apsf.org/article/beach-chair-position-may-decrease-cerebral-perfusion/.
- See, e.g., Kopp C, Anatomy of a Mistake: the Tragic Death of Jessica Santillan, Mar. 16, 2003, online at: https://www.cbsnews.com/news/anatomy-of-a-mistake-16-03-2003.
- See, e.g., Rettner R, Dirty Surgical Instruments Tied to Hundreds of Infections at Colorado Hospital, Lawsuit Alleges, Jun. 20, 2019, at: https://www.livescience.com/65762-dirty-surgical-instruments-infections-lawsuit.html; and, PublicCitizen, Health Letter, Objects Left in the Body After Surgery (Apr. 1, 2013), at: https://www.citizen.org/news/objects-left-in-the-body-after-surgery/.