Suffocation from Over Sedation: Anesthesia Malpractice in Minor Procedures

The purpose of sedation in minor surgeries and medical procedures is, in part, to relieve patient anxiety and to diminish any memory of the event.1 Drugs are given intravenously to sedate and produce a semi-conscious state but not to render the patient unconscious. The patient receiving "conscious sedation" can often respond to verbal cues, and while the patient may fall asleep he or she can easily be woken to respond to caregivers in the room. After the surgery or procedure is over, the patient may be drowsy and will likely have little or no memory of the surgery/procedure.2
What is Conscious Sedation?
Conscious sedation, also known as moderate sedation or "twilight sleep," is usually a combination of pain medication (analgesic or opioid) with a sedative. Sometimes, it may involve a sedative-hypnotic drug. Here are drugs commonly used for conscious sedation:
- Analgesics & Opioids – Demerol, Fentanyl, and/or Morphine
- Sedatives – Valium, Versed, Ativan, and/or Propofol (also a hypnotic)
The effects from these drugs depends on the dose(s) given, and some of them have a narrow margin of safety between the effective dose and the potentially lethal or life-threatening dose. This is known as a narrow therapeutic index (NTI).3 Further, a number of these drugs have the potential to increase the depth of sedation when given together.4 Additionally, people react differently to drugs. For all these reasons, the sedation provider will not always know ahead of time (based on body weight and patient condition) what amount is too little or too much. So, this is where titration and anesthesia monitoring come into play.
During the procedure, the sedation provider should slowly give drugs while monitoring the patient until the desired sedation effect is reached‚ a process known as titration. Also, the sedation provider has to monitor the patient's condition properly, including with the right equipment, and to be alert to changes in deterioration which require different drugs or measures to be employed. All of this process is known as monitored anesthesia care (MAC), which is when conscious sedation is used for diagnostic or therapeutic procedures and is titrated to a level that preserves the ability of patients to breathe on their own and to have airway reflexes.5 The failure of an anesthesia provider, i.e. anesthesiologist or CRNA, to carry out MAC properly, or to correct oversedation when it occurs, can amount to medical malpractice.
What Surgeries or Procedures is it Used For?
Conscious sedation is used for many minor surgeries and endoscopy procedures, including:
- Colonoscopies
- Upper GI Procedures, i.e. EGDs
- Vasectomies
- Biopsies
- Minor Bone Fracture Surgeries
- Cavity Fillings
- Root Canals
- Other Dental Procedures
Advantages of conscious sedation over general anesthesia generally include fewer side effects, faster patient recovery, and shorter facility or hospital stays.
Depth of Sedation
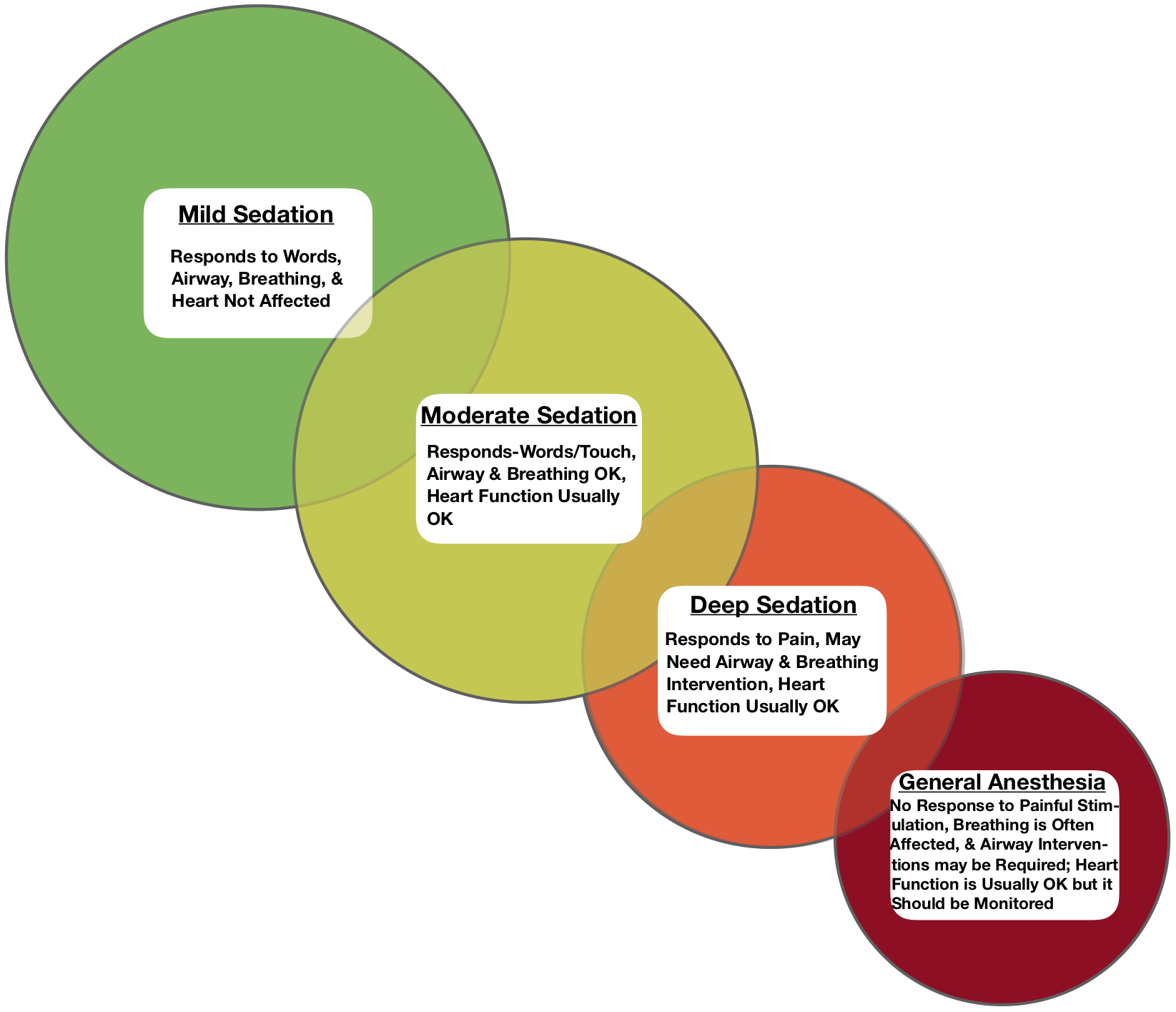
With sedation in minor surgeries and most procedures, the provider usually wants to achieve a moderate, not deep, level of sedation.6 Depth of sedation is actually more of a continuum than it is a discrete level, meaning the patient may be between certain levels. The physiological condition of the patient in the sedation continuum is reflected in the illustration below.7
The Purpose of Monitoring
Various analgesics, opioids, and sedatives used in conscious sedation act on the body by depressing the central nervous system, in particular the breathing centers in the brain. These areas of the brain signal our lungs to breathe and exhale. Additionally, some of these drugs relax the airway muscles and structures, resulting in a loss of airway reflexes.8 The potential for these effects is greater the deeper that the sedation becomes, and some drugs like Propofol are known to cause deep sedation even though only moderate sedation was intended.9 With deep sedation or general anesthesia, life-threatening respiratory depression, airway compromise or obstruction, and/or low blood pressure (hypotension) can occur.10
 Monitoring with anesthesia equipment is how the anesthesia or sedation provider, e.g. anesthesiologist, CRNA, anesthesiologist assistant, or other physician, ensures the patient is at the desired level of sedation and does not experience any serious problem with vital signs, breathing, or physiological condition that can worsen as the level of sedation increases. The sedation process is fluid and the patient's sedation depth can change back-and-forth, especially since some of the drugs are short-acting. If the patient inadvertently reaches a deeper level of sedation than intended, drugs can sometimes be given to reverse that effect.11 Alternatively the physiologic monitoring should promptly identify problems with breathing or the airway if deep sedation or general anesthesia occurs and cannot be immediately lessened, so that the anesthesia provider can intervene for the patient to provide oxygenation and ventilation.
Monitoring with anesthesia equipment is how the anesthesia or sedation provider, e.g. anesthesiologist, CRNA, anesthesiologist assistant, or other physician, ensures the patient is at the desired level of sedation and does not experience any serious problem with vital signs, breathing, or physiological condition that can worsen as the level of sedation increases. The sedation process is fluid and the patient's sedation depth can change back-and-forth, especially since some of the drugs are short-acting. If the patient inadvertently reaches a deeper level of sedation than intended, drugs can sometimes be given to reverse that effect.11 Alternatively the physiologic monitoring should promptly identify problems with breathing or the airway if deep sedation or general anesthesia occurs and cannot be immediately lessened, so that the anesthesia provider can intervene for the patient to provide oxygenation and ventilation.
What Monitoring is Necessary?
The rule for anesthesia providers with conscious sedation is that they must be able to timely support the patients' air movement in and out of the lungs (i.e. ventilation), their oxygenation, and their blood flow (i.e. hemodynamics) if oversedation occurs.12 Pulse oximetry monitoring is the standard way to measure the amount of oxygenation in the blood (SpO2) during conscious sedation but it does not measure ventilation nor does it provide timely notification of changes in ventilation.13 By the same token, just watching to see if the patient's chest moves, i.e. signaling air flow/ventilation, is not a dependable way for the anesthesia provider to make sure there is not apnea or an airway obstruction.14 Since 2011, therefore, the American Society of Anesthesiologists (ASA) has stated that during all anesthetics, adequate ventilation must be ensured by the anesthesia provider in moderate or deep sedation procedures by "monitoring for the presence of exhaled carbon dioxide unless precluded or invalidated by the nature of the patient, procedure, or equipment."15 This means using capnometry equipment when possible to measure the partial pressure of CO2 detected at the end of expiration (i.e. end-tidal CO2) or to display it in graph form (capnography).
Dangers of Oversedation
We inhale air to reach our lungs so the oxygen can be transported in our blood to our organs and tissues. Once the oxygen is depleted and the blood returns, the remaining CO2 is expired from our lungs. Oversedation may result in the interference of adequate oxygenation and ventilation, resulting in a decrease of oxygen (hypoxia), or no oxygen (anoxia), and/or an excess amount of CO2 (hypercarbia) in the blood. This can cause a loss of consciousness, brain injury or death, unless interventions are promptly taken to restore oxygenation and ventilation.
Who is at Greater Risk?
Patients who are at greater risk of suffocation from oversedation are people who are already vulnerable or predisposed. This includes the elderly, people with pre-existing lung, heart or other problems, and those with sleep apnea.16 People who have sleep apnea already have temporary episodes where they stop breathing (apnea) at sleep. So, they can have collapse of the airway with oversedation, and this creates an emergency and need for airway rescue. This is why, when administering conscious sedation drugs, there is even greater reason to monitor sleep apnea patients carefully with capnography/capnometry. With this equipment, many complications such as lack of oxygen to the brain and heart dysfunction can be avoided by early detection and proper treatment.17
When is the Risk Greater?
As noted above, the ASA requires monitoring of end-tidal CO2 when moderate or deep sedation is induced, unless the patient, procedure or equipment prevents the use. Using equipment to measure the CO2 is important because dangerous levels of excess carbon dioxide can build up in the system even though the level of oxygen saturation in the blood is adequate, such as when supplemental oxygen is given.18 The problem is that, unlike hospitals, some surgery centers, medical facilities, and doctors' offices may not have the necessary equipment on hand or personnel available to monitor end-tidal CO2. Likewise, they may not be as well-equipped or as capable as a hospital is to provide an emergency airway, or emergency CPR (code) care if the patient arrests. Additionally, in some procedures where an anesthesiologist is not involved in giving the sedation, the doctor may be less likely to use capnography.19 So, you may face greater risk when a minor surgery or medical procedure is performed with conscious sedation outside of a hospital or without an anesthesiologist, as well as if you have any medical condition that makes you more vulnerable to the effects of oversedation.20
The Lawyer's Role
The lawyer who is experienced in handling anesthesia-related oversedation and medical malpractice cases will know and understand the medicine and important medical literature on this subject. He or she will be able to work with qualified anesthesia expert witnesses as well as other expert consultants to determine and whether, how and why a surgical patient experienced brain injury, arrest, and/or death from oversedation.
Contact Us
The attorneys at Clore Law Group have significant experience and expertise with handling oversedation malpractice cases to successful resolution. We have handled such cases where patients were over sedated and experienced these tragic outcomes as a result of colonoscopy, upper GI (endoscopy), and other minor procedures. If you think that you or a loved one may have experienced a tragic outcome like this from oversedation, you can email us at [email protected], or call us Toll-Free at 1-800-610-2546 for a free and confidential consultation.
Sources
- See, e.g., American Society for Gastrointestinal Endoscopy, Sedation and anesthesia in GI endoscopy, Vol. 87, No. 2, p. 327, Gastro Endosc. (2018), available at: https://www.giejournal.org/article/S0016-5107(17)32111-9/fulltext.
- See American Society of Anesthesiologists (ASA), Sedation Analgesia (2018), which is available at: http://www.asahq.org/lifeline/types%20of%20anesthesia/sedation%20analgesia.
- U.S. Food & Drug Administration (FDA), FY2015 Regulatory Science Research Report: Narrow Therapeutic Index Drugs, found at: https://www.fda.gov/ForIndustry/UserFees/GenericDrugUserFees/ucm500577.htm. See also Overholser BR, Foster DR, Opioid Pharmacokinetic Drug-Drug Interactions, AJMC (Sep. 25, 2011), at: https://www.ajmc.com/journals/supplement/2011/a370_11sep/a370_11sep_overholser_s276tos287 (noting that "[a]s a drug class, opioids are associated with a narrow therapeutic index, wide interindividual variability in response (eg, doses used in an opioid-tolerant patient can be fatal to an opioid-naïve patient), and potentially life-threatening toxicity."); Symington L, Thakore S, A review of the use of Propofol for procedural sedation in the emergency department, Emerg Med J. Vol. 23, No. 2, pp. 89-93 (Feb. 2006)(stating that Propofol is also a NTI).
- FDA Demerol package insert, revealing opioids also have a NTI when combined with CNS depressants: https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/005010s050lbl.pdf; and, Moran TC, Kaye AD, et al, Sedation, Analgesia, and Local Anesthesia: A Review for General and Interventional Radiologists, Radiographics.rsna.org, p. E47 (Mar.-Apr. 2013)(combination of pain & anxiety agents is synergistic).
- See Das S, Ghosh S, Monitored Anesthesia Care: An overview, J Anaesthesiol Clin Pharmacol. Vol. 31, No. 1, pp. 27-29 (Jan-Mar. 2015)(referencing the ASA 2008 Position on monitored anesthesia care).
- See, e.g., Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018: A Report by the American Society of Anesthesiologists Task Force on Moderate Procedural Sedation and Analgesia, the American Association of Oral and Maxillofacial Surgeons, American College of Radiology, American Dental Association, American Society of Dentist Anesthesiologists, and Society of Interventional Radiology, Anesthiol. Vol. 128, No. 3, pp. 437-79 (2018). See also American College of Emergency Physicians (ACEP), Moderate (Conscious) Sedation Frequently Asked Questions, available at: https://sedationcertification.com/moderate-conscious-sedation-frequently-asked-questions/.
- Adapted from ASA, Continuum of Depth of Sedation: Definition of General Anesthesia and Levels of Sedation/ Analgesia (appr. Oct. 24, 2004, amend. Oct. 21, 2009).
- See, e.g., Jones, DR, Salgo P, et al, Conscious Sedation for Minor Procedures in Adults, N Engl J Med., 364;25, p. e54 (June 23, 2011); Blayney MR, Procedural sedation for adult patients: an overview, Cont Educ in Anesthes Cr. Care & Pain, Vol. 12, No. 4, pp. 176-80 (Aug. 2012);
- ASA, Statement on the Safe Use of Propofol (appr. Oct. 27, 2004, amend. Oct. 15, 2014); Beitz A, Riphaus A, et al, Capnographic monitoring reduces the incidence of arterial oxygen desaturation and hypoxemia during propofol sedation for colonoscopy: a randomized, controlled study (ColoCap Study), Am J Gastroent., Vol. 107, No. 8, pp. 1205-12 (2012). In fact, Propofol is often used for deeper sedation and with general anesthesia known as total intravenous anesthesia (TIVA). See, e.g., Miller TE, Gan TJ, Total Intravenous Anesthesia and Anesthetic Outcomes, J Cardiothor & Vasc Anesth. Vol. 29, No S1, pp. S11-S15 (June 2015).
- Id. See also Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018, n6, at 438, 442; Bhananker SM, Poser KL, et al, Injury and liability associated with monitored anesthesia care: a closed claims analysis, Anesth. Vol. 104, No. 2, pp. 228-34 (Feb. 2006); Jones, DR, Salgo, P, et al, Conscious Sedation for Minor Procedures in Adults, N Engl J Med., 364;25, p. e54 (June 23, 2011).
- Dahan A, Aarts, L, et al, Incidence, Reversal, and Prevention of Opioid-induced Respiratory Depression, Anesthesiol., Vol. 112, No. 1, pp. 226-38 (Jan. 2010); ASA, Practice Guidelines for Sedation and Analgesia by Non-Anesthesiologists, Anesthesiol. Vol. 96, No. 4, pp. 1004-17 (Apr. 2002)(also noting at 1011-12 that there are no specific reversal agents for the deeper sedation drugs Propofol, Ketamine, or Methohexital).
- Jones, DR, Salgo, P, et al, n10, at e54-55. See generally Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018, n6.
- Physio-Control, Inc., ASA Upgrades Procedural Sedation Standards: Requirement for Capnography, which is available at: https://www.physio-control.com/WorkArea/DownloadAsset.aspx?id=2147486279 (quoting from Lightdale JR. Microstream Capnography Improves Patient Monitoring During Moderate Sedation: A Randomized, Controlled Trial, Pediatr. Vol. 117, No. 6, pp. e1170-e1178 (June 2006)).
- ASA, Statement on the Safe Use of Propofol, n9, at 1.
- ASA, Standards for Basic Anesthesia Monitoring, Std. 3. Ventilation, 3.2.4 (eff. July 1, 2011, aff'd. Oct. 28, 2015). Note, however, that the American Society of Gastrointestinal Endoscopy (ASGE) recommends but does not require the use of capnography during deep sedation. ASGE Standards of Practice Committee, Guidelines for sedation and anesthesia in GI Endoscopy, Gastroint Endosc., Vol. 87, No. 2, pp. 327-37 (2018), at 333, 335.
- See, e.g., Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018, n6, at 440; Das S, Monitored Anesthesia Care, n5, at 28; ASA, Practice Guidelines for the Perioperative Management of Patients with Obstructive Sleep Apnea, Anesthesiol. Vol. 120, No. 2, pp. 1081-93 (Feb. 2014).
- Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018, n6, at 442; Beitz A, et al, n9.
- See, e.g., Gerstenberger PD, Capnography and Patient Safety for Endoscopy, Clin Gastroenterol & Hepat. Vol. 8, No. 5, pp. 423-25 (2010).
- While the national practice guidelines for anesthesiologists, for oral and maxillofacial surgeons, and for dentists assistants all "strongly agree" with the recommendation to use capnography monitoring in moderate sedation procedures, the national guidelines for gastroenterologists only suggest capnography be considered in endoscopic procedures where deep sedation is targeted. See Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018, n6, at 442; cf., ASGE Guidelines for sedation and anesthesia, n17, at 333, 335 (2018). Yet those same gastroenterology guidelines also recommend sedation be administered by an "anesthesia provider" (i.e. anesthesiologist or nurse anesthetist) rather than the endoscopist (i.e. gastroenterologist) when the patient is "at risk for airway compromise." Id. at 335.
- Id.; Metzner J, Posner KL, et al, The risk and safety of anesthesia a remote locations: the US closed claims analysis, Curr Opin Anaesthesiol., Vol. 22, No. 4, pp. 502-08 (Aug. 2009); Cravero JP, et al, Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room: report from the Pediatric Sedation Research Consortium. Pediatr. Vol. 118, pp. 1087-96 (2006).