Propofol Misuse, Monitoring, and Medical Malpractice

When pop music icon Michael Jackson died from "acute propofol intoxication,"1 the dangers of a drug with which the general populace had little knowledge came to light. Propofol is a powerful sedative-hypnotic drug used by anesthesia providers for deep sedation procedures and general anesthesia in surgery.2 The drug is one that is used daily for these purposes, for procedures and surgeries throughout the world. The benefits of propofol over other drugs include faster recoveries, i.e. rapid recovery from anesthesia and the ability to move around soon after surgery, less nausea and vomiting after surgery, and overall greater patient satisfaction.3 On the other hand, propofol misuse can be extremely dangerous if not given in a monitored environment like surgery, as we saw with Michael Jackson; this can amount to medical malpractice. A few years later, famous comedian Joan Rivers died from the effects of propofol during a routine, elective endoscopic procedure on her vocal cords; and we learned that the drug can be just as deadly in the operating room when it causes oversedation and abnormal vital signs that are not timely detected and corrected. These circumstances may also constitute medical malpractice.4 Propofol was originally developed for general anesthesia, as an alternative to other drugs.5 The brand name of propofol is Diprivan. Propofol has been referred to as the "milk of amnesia" because of milky-like appearance of the drug when it is prepared to be given via intravenous injection.6 While propofol is safe and effective when properly used and given, there are five reasons that it can be dangerous even in minor medical procedures and surgeries. The drug: (1) has a narrow therapeutic index, (2) can easily cause a deeper level of sedation than is intended, (3) can cause airway compromise or profound cardiorespiratory dysfunction in patients who are already vulnerable to those conditions (e.g. sleep apnea, heart/lung and other preexisting conditions), (4) requires continual and specialized monitoring, including of blood oxygen and expired carbon dioxide levels, as well as prompt intervention to correct these problems, and (5) has no antidote (i.e. reversal drug).
Propofol Has a Narrow Therapeutic Index (NTI)
Most people do not realize certain drugs have a fine line between the risks they present and benefits they confer. These drugs are referred to in the health care field as "narrow therapeutic index" (NTI) drugs, meaning they have a narrow margin of safety between the effective dose and the potentially lethal dose. As a result, small differences in dose or blood concentrations of these drugs can therefore have life-threatening differences in the effects on patients.7 NTI drugs are thus more commonly associated with drug-related problems in the hospital setting than are non-NTI drugs.8 Propofol has long been recognized to be an NTI drug.9
Propofol Can Cause Oversedation
People react differently to drugs, and the anesthesia provider will not always know ahead of time (based on body weight and patient condition) what amount is too little or too much. Propofol is a drug which is well known to sometimes rapidly cause deeper levels of sedation than the anesthesia provider intends. Additionally, there is greater likelihood of deeper than intended sedation with greater amounts of propofol, particularly when combined with other sedatives. Because of these facts, the American Society of Anesthesiologists (ASA) and the American Association of Nurse Anesthetists (AANA) say that drugs like propofol require "special attention."10 The ASA also states that anesthesia providers should, when using Propofol, provide monitoring and care for deep sedation even though only moderate sedation is planned for the procedure or surgery.11 Further, deep levels of sedation can also reach the point of general anesthesia, where patients often needs airway intervention to help them breathe, and their heart function may also be impaired.12
Propofol Can Exacerbate Airway, Heart and/or Lung Problems
Propofol lowers blood pressure, and high rates of infusion also significantly decrease the heart rate. Common side effects may also include periods where breathing stops (apnea).13 These effects are more likely to occur when larger doses are rapidly given, and in debilitated or elderly patients.14 This is because people who are already prone or susceptible to heart, lung or airway problems can experience a worsening of those problems with propofol. This is especially true for people who have obstructive sleep apnea (OSA), where structures in the throat (soft palate and uvula) usually fall or sag into the airway, thus blocking it, while sleeping. Normally, the person with OSA only has transient apnea‚ meaning they stop but then resume breathing
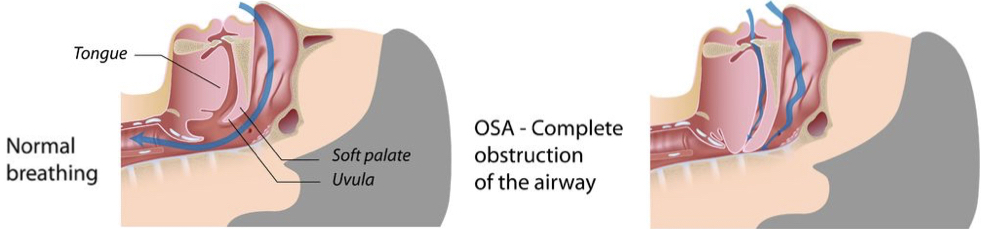
(and sometimes awake) after temporary periods of apnea. With propofol, however, the condition may become more pronounced and, if the person is in a deep level of sedation, the body's natural drive to resume breathing becomes diminished.
Propofol Requires Careful and Proper Monitoring & Intervention
 When propofol is administered, the anesthesia provider has to monitor the patient's condition properly, including with the right equipment, and to be alert to cardiorespiratory deterioration which may require different drugs or measures to be employed. Likewise, the anesthesia caregiver has to be on the lookout for signs of apnea, which may require airway support or intervention like intubation (i.e. insertion of breathing tube). All of this process is known as monitored anesthesia care (MAC), which is when conscious sedation is used for diagnostic or therapeutic procedures and is titrated (meaning slowly-given to reach the desired level) while preserving the ability of patients to breathe on their own and to have airway reflexes.15 Propofol manufacturers warn that the drug should only be given by persons trained to administer anesthesia, and not by those actually performing the diagnostic or surgical procedure.16 The ASA further states that propofol requires monitoring for not just the levels of oxygen in the blood but also the build-up of carbon dioxide (CO2) in the movement of air out of the lungs.17 This is called capnometry or capnography. The reason for capnometry or capnography monitoring is to identify more quickly the blocked airway when propofol is used.
When propofol is administered, the anesthesia provider has to monitor the patient's condition properly, including with the right equipment, and to be alert to cardiorespiratory deterioration which may require different drugs or measures to be employed. Likewise, the anesthesia caregiver has to be on the lookout for signs of apnea, which may require airway support or intervention like intubation (i.e. insertion of breathing tube). All of this process is known as monitored anesthesia care (MAC), which is when conscious sedation is used for diagnostic or therapeutic procedures and is titrated (meaning slowly-given to reach the desired level) while preserving the ability of patients to breathe on their own and to have airway reflexes.15 Propofol manufacturers warn that the drug should only be given by persons trained to administer anesthesia, and not by those actually performing the diagnostic or surgical procedure.16 The ASA further states that propofol requires monitoring for not just the levels of oxygen in the blood but also the build-up of carbon dioxide (CO2) in the movement of air out of the lungs.17 This is called capnometry or capnography. The reason for capnometry or capnography monitoring is to identify more quickly the blocked airway when propofol is used.
Propofol Has No Antidote
As with certain other deep sedation drugs, propofol has no specific reversal agent or antidote.18 So, the anesthesia provider or caregiver administering propofol must plan ahead for what drugs and measures will be employed in the event any of these dangerous side-effects are detected by timely and proper monitoring.
Dangers of Propofol Medical Malpractice
We inhale air to reach our lungs so the oxygen can be transported to our organs and tissues. Once the oxygen is depleted, the remaining CO2 is expired from our lungs. Suffocation, also known as asphyxiation, from the effects of propofol can result when the airway is blocked and apnea occurs for too long. This can cause an almost immediate loss of consciousness, and while the heart continues to beat for a short period of time, brain injury followed by death will occur in minutes unless interventions are taken to rescue the patient by restoring ventilation (i.e. air movement in and out of the lungs). This is why the ASA requires propofol providers to have the knowledge, skills and equipment to be able to "rescue" the patient from general anesthesia, as well as to be able to identify and manage airway and cardiovascular deterioration (e.g. low blood pressure, low heart rate, etc.).19 Danger from Diprivan can occur whenever the propofol giver does not perform timely and proper monitoring, or if he or she becomes preoccupied with the procedure instead of the patient's condition. Likewise, if the propofol provider ignores preexisting heart, lung, or airway vulnerability of his or her patient, then the dangers with propofol may be even more pronounced. In short, while propofol can be safe drug which provides several benefits for patients having surgery or medical procedures, it is equally true that the "milk of amnesia" can be deadly when it is not cautiously used, when the patient is not carefully monitored, or when the patient is not quickly rescued from the effects of over sedation. All of these situations can arise due to medical malpractice.
The Lawyer's Role
The lawyer who is experienced in handling propofol cases will know and understand the medicine and important medical literature on this subject. He or she will be able to work with qualified anesthesia expert witnesses as well as other expert consultants to determine and whether, how and why a patient receiving propofol or other drugs during a medical or surgical procedure experienced brain injury, arrest, and/or death. In short, the lawyer's will be able to investigate and determine if propofol oversedation caused such a tragedy, as well as to prosecute for medical malpractice if it did.
Contact Us
The attorneys at Clore Law Group have significant experience and expertise with handling propofol and other drug mismanagement and medical malpractice cases to successful resolution. We have handled such cases where patients were over sedated with propofol during colonoscopy and EGD (upper GI) procedures. If you think that you or a loved one may have experienced a tragic outcome like this from propofol, you can email us at [email protected], or call us Toll-Free at 1-800-610-2546 for a free and confidential consultation.
Sources
- See https://latimesblogs.latimes.com/lanow/2009/08/michael-jackson-3.html. See also the following stories: https://www.scientificamerican.com/article/propofol-michael-jackson-doctor, and https://www.medicinenet.com/script/main/art.asp?articlekey=113188.
- See, e.g., https://www.verywellhealth.com/what-is-diprivan-3157312.
- White PF, Propofol: It's Role in Changing the Practice of Anesthesia, Anesthesiol. Vol. 109, No. 6, pp. 1132-36 (Dec. 2008); Otto MA, Colonoscopy patients prefer propofol over fentanyl/midazolam, American College of Surgeons (ACS) Surgery News (June 29, 2017).
- See https://www.beckershospitalreview.com/quality/medical-standards-of-care-and-the-joan-rivers-death.html.
- White PF, Propofol: It's Role in Changing the Practice of Anesthesia, n3, at 1135.
- Euliano TY, Gravenstein, JS, Essential Anesthesia: From Science to Practice, p. 173 (Cambridge Univ. Press 2005).
- FDA, FY2015 Regulatory Science Research Report: Narrow Therapeutic Index Drugs
- Blix HS, Viktil KK, et al, Drugs with narrow therapeutic index as indicators in the risk management of hospitalized patients, Pharm Pract. Vol. 8, No. 1, pp. 50-55 (Jan-Mar. 2010); see also 21 CFR 320.33(c)(incorporating this definition in the FDA bioequivalence criteria).
- See Blayney, MR, Procedural sedation for adult patients: an overview, Cont'g Educ in Anesth, Crit. Care & Pain, Vol 12, No. 4, pp. 176-80, at 177 (Apr. 2012); Repici A, Pagano N, et al, Balanced propofol sedation administered by nonanesthesiologists: The first Italian experience, World J. Gastroenterol. Vol. 17, No. 33, pp. 3818-23 (Sep. 7, 2011).
- American Association of Nurse Anesthetists (AANA) and American Society of Anesthesiologists (ASA), AANA-ASA Joint Position Statement Regarding Propofol Administration (adopted Apr. 14, 2004).
- ASA, Statement on the Safe Use of Propofol (appr. Oct. 27, 2004, amend. Oct. 15, 2014); Beitz A, Riphaus A, et al, Capnographic monitoring reduces the incidence of arterial oxygen desaturation and hypoxemia during propofol sedation for colonoscopy: a randomized, controlled study (ColoCap Study), Am J Gastroent., Vol. 107, No. 8, pp. 1205-12 (2012). In fact, propofol is often used for deeper sedation and with general anesthesia known as total intravenous anesthesia (TIVA). See, e.g., Miller TE, Gan TJ, Total Intravenous Anesthesia and Anesthetic Outcomes, J Cardiothor & Vasc Anesth. Vol. 29, No S1, pp. S11-S15 (June 2015).
- ASA, Continuum of Depth of Sedation: Definition of General Anesthesia and Levels of Sedation/ Analgesia (appr. Oct. 24, 2004, amend. Oct. 21, 2009).
- Bilotta F, Fiorani L, et al, Cardiovascular effects of intravenous Propofol administered at two infusion rates: a transthoracic echocardiographic study, Anesth. Periop med, Crit. Care & Pain (Assoc. of Anesthetists, Aug. 6, 2008); see also https://www.rxlist.com/propofol-side-effects-drug-center.html.
- See, e.g., Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018: A Report by the American Society of Anesthesiologists Task Force on Moderate Procedural Sedation and Analgesia, the American Association of Oral and Maxillofacial Surgeons, American College of Radiology, American Dental Association, American Society of Dentist Anesthesiologists, and Society of Interventional Radiology, Anesthiol. Vol. 128, No. 3, pp. 437-79, at 440 (2018); Das S, Ghosh S, Monitored Anesthesia Care: An overview, J Anaesthesiol Clin Pharmacol. Vol. 31, No. 1, pp. 27-29, at 28 (Jan-Mar. 2015); ASA, Practice Guidelines for the Perioperative Management of Patients with Obstructive Sleep Apnea, Anesthesiol. Vol. 120, No. 2, pp. 1081-93 (Feb. 2014). See also propofol label information: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=28d7ba00-f824-4e55-139a-03f509c099db.
- See Das S, Ghosh S, Monitored Anesthesia Care: An overview, n15, at 27-29 (referencing the ASA 2008 Position on monitored anesthesia care).
- ASA, Statement on the Safe Use of Propofol, n11, at 1-2.
- Id. at 1. Also note that the national practice guidelines for oral and maxillofacial surgeons, and for dentists assistants, also "strongly agree" with the recommendation to use capnography monitoring in moderate sedation procedures, but the national guidelines for gastroenterologists only suggest capnography be considered in endoscopic procedures where deep sedation is targeted. See Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018, n6, at 442; cf., ASGE Guidelines for sedation and anesthesia, n17, at 333, 335 (2018). Yet those same gastroenterology guidelines also recommend sedation be administered by an "anesthesia provider" (i.e. anesthesiologist or nurse anesthetist) rather than the endoscopist (i.e. gastroenterologist) when the patient is "at risk for airway compromise." Id. at 335.
- ASA, Practice Guidelines for Sedation and Analgesia by Non-Anesthesiologists, Anesthesiol. Vol. 96, No. 4, pp. 1004-17 (Apr. 2002)(noting at 1011-12 that there are no specific reversal agents for the deeper sedation drugs Propofol, Ketamine, or Methohexital).
- ASA, Statement on the Safe Use of Propofol, n11.