Who is Giving the Gas? Brain Injury & Death from Anesthesia Malpractice

There is an old adage told by physicians that when patients are going to have surgery, they want to know who will be performing the operation, but when doctors are about to have surgery on themselves their first question is always, "Who is giving the gas?"1 The adage underscores the significance of the role of the anesthesia provider in surgery, and the potential for life-threatening medical malpractice that can occur in relation to general anesthesia and the monitoring of effects of anesthetics.
Anesthesia Provider's Role
 Anesthesia providers, i.e. anesthesiologists, anesthesiologist assistants, and certified registered nurse anesthetists (CRNAs), are responsible for determining which general anesthetics to give a patient in surgery as well as the monitoring of the patient's vital signs, breathing, and physiological condition during the surgery. Serious errors can arise not only if the wrong drugs (e.g. anesthetics, narcotics, opioids, sedatives, hypnotics, and/or inhaled gases, etc.), combinations, or amounts are given but also if the patient's airway is compromised before surgery begins, or his or her breathing is compromised during the surgery. The movement of air in and out of the lungs is called ventilation. It has long been recognized that most case of anesthesia medical malpractice resulting in brain injury or, if severe enough, death, invariably arise due to a severe lack of oxygen, i.e. anoxia, because of problems with ventilation or the airway.2
Anesthesia providers, i.e. anesthesiologists, anesthesiologist assistants, and certified registered nurse anesthetists (CRNAs), are responsible for determining which general anesthetics to give a patient in surgery as well as the monitoring of the patient's vital signs, breathing, and physiological condition during the surgery. Serious errors can arise not only if the wrong drugs (e.g. anesthetics, narcotics, opioids, sedatives, hypnotics, and/or inhaled gases, etc.), combinations, or amounts are given but also if the patient's airway is compromised before surgery begins, or his or her breathing is compromised during the surgery. The movement of air in and out of the lungs is called ventilation. It has long been recognized that most case of anesthesia medical malpractice resulting in brain injury or, if severe enough, death, invariably arise due to a severe lack of oxygen, i.e. anoxia, because of problems with ventilation or the airway.2
Anesthesia Medical Malpractice
The American Society of Anesthesiologists (ASA) reported between 1985 and 2004, as part of its projects studying anesthesia errors forming the basis of medical malpractice claims and settlements, on the incidence of errors related to serious claims such as brain injury and death.3 The eight categories of errors recognized were:
- Inadequate Ventilation – i.e. inadequate provision of oxygen (O2) and/or removal of expired gases (CO2) from the lungs during surgery.
- Esophageal Intubation – i.e. erroneous insertion of the breathing (endotracheal/ET) tube into the food pipe (esophagus) leading to the stomach instead of the airway connection the lungs.
- Airway Obstruction – i.e. causing or failing to correct an obstruction of the airway.
- Bronchospasm – i.e. causing or failing to correct a tightening of the muscles (bronchi) that line the lung airways.
- Difficult Intubation – i.e. causing the airway to be difficult to intubate, such as with repeated failed attempts at intubation, or failing to recognize in advance the difficulty of intubation.
- Aspiration – i.e. causing (with the wrong anesthetics) or failing to timely respond to vomiting of stomach contents into the lungs.
- Premature Extubation – i.e. early removal of the endotracheal tube.
- Others – i.e. concerning the lungs or airway.
The pie chart identifies the percentages of each of these respiratory events for the total of all such claims from the 1970's through the 1990's based on the ASA Closed Claims Project.4
Most Common Cases of Medical Malpractice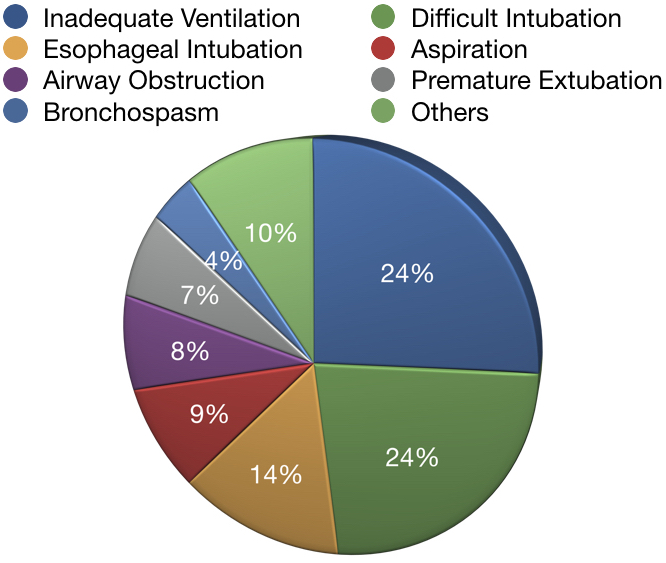
Of the eight categories of serious anesthesia errors, the three most common ones are inadequate ventilation, esophageal intubation, and difficult intubation. These errors have resulted in the largest claims and payments/settlements due to death or permanent brain damage,5 and often are related to "situational awareness" errors by the anesthesia provider—in terms of failing to perceive information, comprehend its meaning, or to anticipate or plan.6
Inadequate Ventilation
During surgery, the anesthesia provider has to monitor the patient's condition properly, including with the right equipment, and to be alert to changes in deterioration which require different drugs or measures to be employed. When general anesthesia is administered through a mask or IV medication in a vein, the patient will reach such a deep level of unconsciousness that the brain does not respond to pain signals or reflexes, and breathing slows significantly. Patients' airways often need to be secured in some fashion once general anesthesia begins, in order to 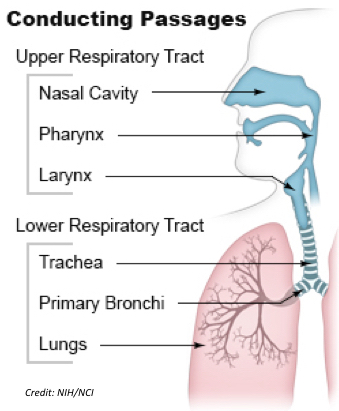 maintain the airway in the upper respiratory tract and to provide for ventilation to and from the lower respiratory tract. To determine if ventilation is adequate during general anesthesia, certain monitoring is performed. The monitor or anesthesia machine is used to determine if an adequate amount of oxygen is going into the lungs to breathe for the patient, and that a proper amount of CO2 is coming out of the lungs once the O2 is depleted. The required monitoring with general anesthesia to assess the levels of oxygenated blood in circulation is known as pulse oximetry7: it measures blood oxygen saturation levels or SpO2. If you have been in the hospital and at some point had clothespin-like clip device attached to your finger, it was for this purpose. In addition to knowing the amount of oxygen in circulating blood, it is also important for the anesthesia provider to know if the lungs are retaining excess carbon dioxide (CO2). With general anesthesia, the required equipment to monitor CO2 is called capnometry (number measurement) or capnography (graph measurement)8: capnometry analyzes and measures the partial pressure of CO2 detected at the end of exhalation, i.e. called end-tidal CO2. The failure to continually assess and respond to problems with either O2 intake or CO2 output can result in lack of oxygen to the brain and/or excess carbon dioxide build-up that can also damage the brain. Hence, inadequate oxygenation and ventilation may result in brain injury and/or death
maintain the airway in the upper respiratory tract and to provide for ventilation to and from the lower respiratory tract. To determine if ventilation is adequate during general anesthesia, certain monitoring is performed. The monitor or anesthesia machine is used to determine if an adequate amount of oxygen is going into the lungs to breathe for the patient, and that a proper amount of CO2 is coming out of the lungs once the O2 is depleted. The required monitoring with general anesthesia to assess the levels of oxygenated blood in circulation is known as pulse oximetry7: it measures blood oxygen saturation levels or SpO2. If you have been in the hospital and at some point had clothespin-like clip device attached to your finger, it was for this purpose. In addition to knowing the amount of oxygen in circulating blood, it is also important for the anesthesia provider to know if the lungs are retaining excess carbon dioxide (CO2). With general anesthesia, the required equipment to monitor CO2 is called capnometry (number measurement) or capnography (graph measurement)8: capnometry analyzes and measures the partial pressure of CO2 detected at the end of exhalation, i.e. called end-tidal CO2. The failure to continually assess and respond to problems with either O2 intake or CO2 output can result in lack of oxygen to the brain and/or excess carbon dioxide build-up that can also damage the brain. Hence, inadequate oxygenation and ventilation may result in brain injury and/or death
Intubation Problems
Prior to surgery, anesthesia providers conduct a preanesthetic evaluation or assessment. Part of the assessment is to determine details of the patient's physical condition or history of allergies that might result in complications from anesthesia, as well as when the patient last ate; the latter concern determines what type of drugs are safe for the patient so as to prevent inadvertent aspiration during anesthesia. A significant part of the evaluation, however, is to assess the patient's airway for the placement of a supraglottic airway or endotracheal tube before the operation involving general anesthesia begins.
Difficult Intubation
 The airway assessment is made to predict the ease of intubation, and while there is really no perfect airway assessment tool, the Mallampati (named for the doctor who created it) airway classification is commonly used as one of the bedside screening tests to evaluate the ease of direct laryngoscopy--i.e. the airway visual examination before the tube is inserted. With direct laryngoscopy, a metal blade is used to move the tongue out of the way and see the structures inside to estimate the difficulty of intubation. Although many difficult intubations are often unexpected, an airway exam should be performed, if possible. Failure to perform an airway evaluation or to use the proper airway equipment, or to avoid multiple unnecessary intubation attempts (in elective surgeries if the airway becomes compromised during attempted intubation), may lead to complications such as failure to oxygenate and ventilate. There are several methods to place a breathing tube (endotracheal tube or ET tube) into your windpipe, including by both direct and indirect laryngoscopy with a flexible scope. With repeated unsuccessful intubation attempts, bleeding in or swelling of the airway can occur. If the bleeding or swelling is significant, it can result in a situation where the airway closes off and neither the tube can be inserted into the trachea nor can the expired CO2 be released from the lungs‚ so-called "cannot intubate or ventilate" situation. This may result in the need for an emergency surgical airway to be made in the front of the neck (cricothyrotomy or tracheostomy). In sum, the failure to predict and respond timely and properly to the difficult airway can also result in brain injury or death.
The airway assessment is made to predict the ease of intubation, and while there is really no perfect airway assessment tool, the Mallampati (named for the doctor who created it) airway classification is commonly used as one of the bedside screening tests to evaluate the ease of direct laryngoscopy--i.e. the airway visual examination before the tube is inserted. With direct laryngoscopy, a metal blade is used to move the tongue out of the way and see the structures inside to estimate the difficulty of intubation. Although many difficult intubations are often unexpected, an airway exam should be performed, if possible. Failure to perform an airway evaluation or to use the proper airway equipment, or to avoid multiple unnecessary intubation attempts (in elective surgeries if the airway becomes compromised during attempted intubation), may lead to complications such as failure to oxygenate and ventilate. There are several methods to place a breathing tube (endotracheal tube or ET tube) into your windpipe, including by both direct and indirect laryngoscopy with a flexible scope. With repeated unsuccessful intubation attempts, bleeding in or swelling of the airway can occur. If the bleeding or swelling is significant, it can result in a situation where the airway closes off and neither the tube can be inserted into the trachea nor can the expired CO2 be released from the lungs‚ so-called "cannot intubate or ventilate" situation. This may result in the need for an emergency surgical airway to be made in the front of the neck (cricothyrotomy or tracheostomy). In sum, the failure to predict and respond timely and properly to the difficult airway can also result in brain injury or death.
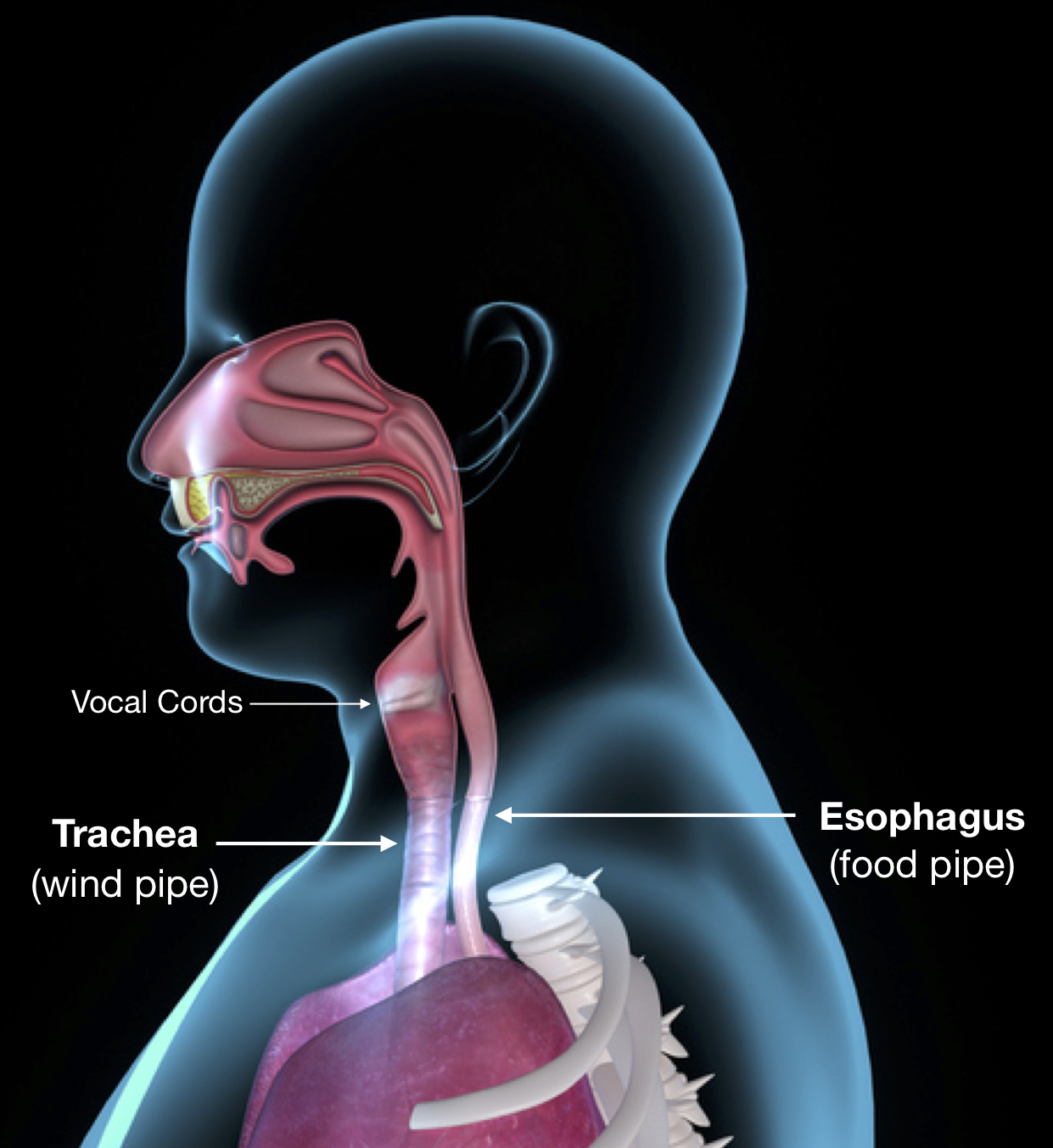 Esophageal Intubation
Esophageal Intubation
The ASA has examined all three of these catastrophic respiratory events in relation to whether the anesthesia provider monitored the patient's SpO2 or CO2 during surgery, and found that where there were inadequate ventilation or intubation problems, more injuries and claims arose when end tidal CO2 or capnometry/ capnography monitoring was not utilized, as seen in the charts on the right.10
The Lawyer's Role
The Clore Law Group attorneys have seen numerous errors involving anesthesia where breathing was improperly compromised and/or not timely recognized during surgery. These cases include inadequate ventilation, intubation problems, difficult intubation, "cannot intubate or ventilate" situations, aspiration, etc. We work with highly qualified anesthesiologists and other experts in these fields to determine and establish what went wrong, why and how in terms of anesthesia mishaps. And we have had significant past success in prosecuting anesthesia mishaps to substantial settlement.
Contact Us
If you are concerned that your loved one or family member could have possibly experienced brain injury or death due to some anesthesia mishap or medical malpractice in a healthcare setting, you can email us at [email protected], or call us Toll Free at 1-800-610-2546 for a free and confidential consultation.
Sources
- The adage refers to general anesthesia of the deepest type, which in the past mainly involved induction by inhaled gases. Over the past twenty years, however, induction via total intravenous anesthesia (TIVA) drugs has become a popular way to achieve general anesthesia. See, e.g., Total Intravenous Anesthesia and Anesthetic Outcomes, J. Cardiothor & Vasc Anesthes., Vol. 29, No. S1, pp. S11-S15 (June 2015). Improper use of TIVA or lack of appropriate monitoring can also cause brain injury or death from oversedation, including from drugs like propofol.
- Ruth HS, Haugen FP, et al, Anesthesia Study Commission: findings of eleven years' activity, JAMA Vol. 135, p. 881 (1947); Becher HK, Todd DP, A study of the deaths associated with anesthesia and surgery based on a study of 599,548 anesthesia in ten institutions, 1948-1952, inclusive, Ann Surg. Vol. 140, pp. 2-35 (1954); Utting JE, Gray TC, et al, Human misadventure in anesthesia, Can Anaesth Soc J. Vol. 26 p. 472 (1979); Cooper JB, Newbower RS, et al, Preventable anesthetic mishaps: a study of human factors, Anesthes. Vol. 49, p. 399 (1978), Russell WJ, Webb RK, et al, Problems with ventilation: an analysis of 2000 incident reports, Anaesth Intens. Care Vol. 21, p. 617 (1993); Harrison GC, Death attributable to anesthesia: a ten-year survey, 1967-1976, Br J Anaesth. Vol. 50, p. 1041 (1978); Holland R, Anesthesia-related mortality in Australia, Int Anesthesiol Clin. Vol. 22, p. 61 (1984); Keenan RL, Boyan CP, Cardiac arrest due to anesthesia: a study of incidence and causes, JAMA Vol. 253. P. 2373 (1985); Tiret L, Desmonts JM, et al, Complications associated with anesthesia: a prospective survey in France, Can Anaesth Soc J. Vol. 33, p. 336 (1986).
- Benumof JL, Airway Management: Principles and Practice, p. 945 (Mosby-Year Book, 1996); Hagberg, CA, Benuomoff's Airway Management, Ch. 53, p. 1273 (2d ed. 2007).
- Adapted from Hagberg, n2, Table 53-3, at 1274-75.
- Id. at Table 53-4, at 1275 (displaying data from the ASA Closed Claims Project of 2002).
- Schulz CM, Burden A, et al, Frequency and Type of Situational Awareness Errors Contributing to Death and Brain Damage: A Closed Claims Analysis, Anesthes. Vol. 127, No. 2, pp. 326-337 (Aug. 2017).
- American Society of Anesthesiologists (ASA), Standards for Basic Anesthetic Monitoring, Std. II, 2.1 Oxygenation (eff. July 1, 2011).
- Id. at 3, Ventilation, 3.2.1-3.2.2.
- Hornardar MR, Posner KL, et al, Delayed Detection of Esophageal Intubation in Anesthesia Malpractice Claims: Brief Report of a Case Series, Anesth Analg., Vol. 125, No. 6, pp. 1948-51 (Dec. 2017).
- Adapted from the ASA Closed Claims Project of 2002, Fig. 4; see also Schulz, n5, at 331 (noting that such lack of O2/CO2 monitoring resulted in errors of perception, i.e. failure to recognize the declining respiratory status of patients often until after cardiac arrest.).