Unnecessary Surgery: When the Doctor Gambles, Who Puts Up the Stakes?

The fundamental question for a surgeon who recommends an operation is whether the potential benefits outweigh the known risks. Surgery carries risks. We all know that. The question is how badly does the person need surgery, and what are the risks (and severity of risks) of complications that can happen? When the risk of serious complications exceed the risk of potential benefits, common sense tells us that surgery is not a wise choice. So, why do doctors still recommend and order unnecessary surgeries in this day and age? It would be comforting to us to think that surgeons do this purely for altruistic reasons, based on a belief that hope should transcend fear. But medicine depends on evidence-based outcomes, not hope or fear. Sadly, the truth of why most unnecessary surgeries occur is not because of the surgeons' hope, nor the patient's fear; the reasons, as will be discussed, commonly have to do with surgeons' personal interests taking precedence over the patients' personal interests.
How Common are Unnecessary Surgeries?
More than half a century ago, the Director of the American College of Surgeons remarked that "the public would be shocked if it knew the amount of unnecessary surgery performed . . . ."1 By 1976, the American Medical Association (AMA) called for a congressional hearing on the subject, claiming there were around "2.4 million unnecessary operations performed [annually] on Americans at a cost of $3.9 billion and that 11,900 patients had died from unneeded operations."2 Fast-forward to the present, and it is a sad reality that even though unnecessary surgeries are considered "never events" (meaning they should never occur), over 11% of all surgeries are felt to be unnecessary. In short, unnecessary surgeries are still being performed every day our country.3
When is Surgery Unnecessary?
Unnecessary surgery has been defined as "any surgical intervention that is either not needed, not indicated, or not in the patient's best interest when weighed against other available options, including conservative measures."4
What are the Most Common Unnecessary Surgeries?
The most common unneeded operations each year in the U.S. are the following5:
- heart stents
- pacemakers
- back (spine) surgeries
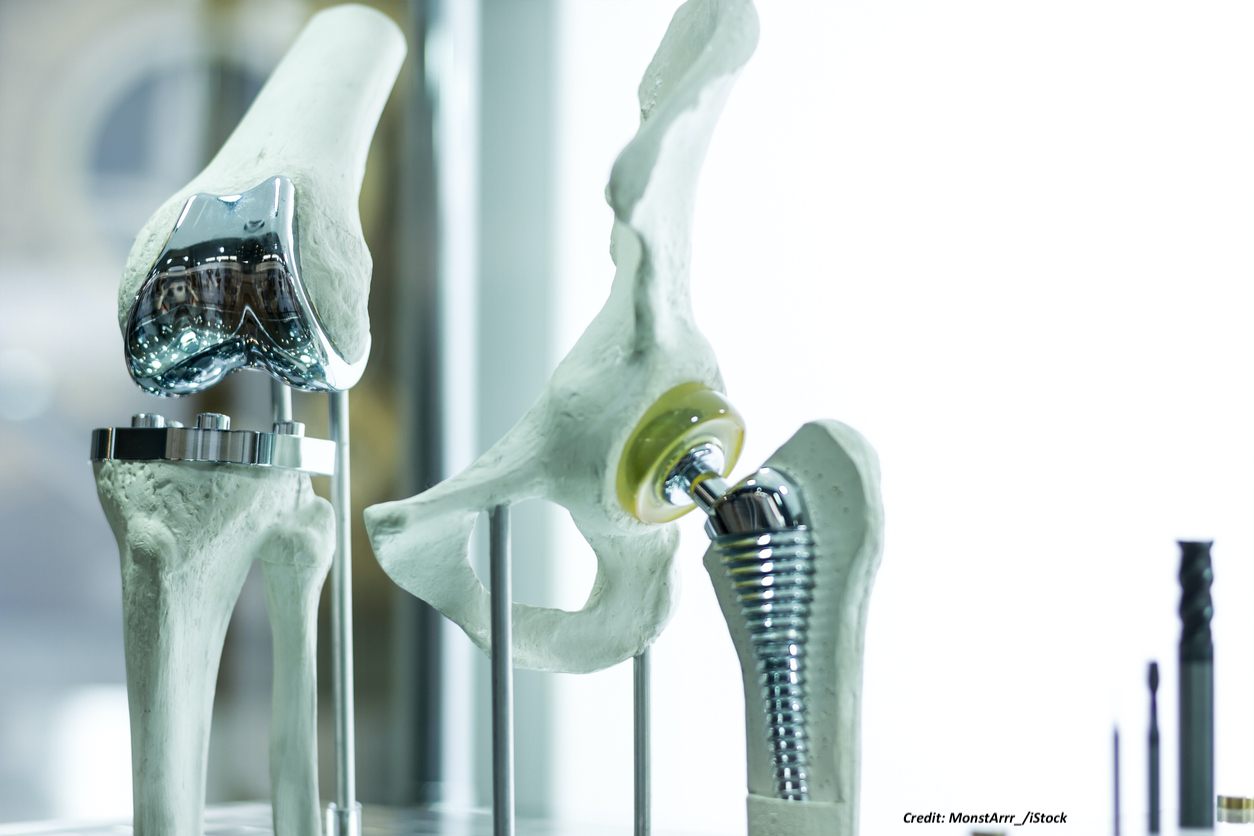
- knee and hip surgeries
- hysterectomies
- radical prostatectomy
- gallbladder removal
- Cesarean sections
- tonsillectomies
What is the Harm from Unnecessary Surgeries?
If the patient recovers well after surgery, and his or her insurance company does not catch the unnecessary surgery error, it may never come to light. And, the surgeon who performed the operation can always claim, "no harm, no foul" even if it is later discovered. But when something goes wrong, as in the thousands of cases where patients die, are injured, or are made to suffer for their entire lives,6 the story is far different. In lawsuits involving surgery where a medical complication has occurred, surgeons and their lawyers are quick to disclaim responsibility for the risks of surgery. They often point out that the patient signed a consent form beforehand, and therefore he/she knew of the risks of complications that could occur with surgery but chose to have it anyway.
Yet when the surgery is alleged to be unnecessary, surgeons and their lawyers may instead claim that the complication could have happened even without surgery, or (in cases where only minor injury occurred) that the complication was not that significant. So, excuses for unnecessary surgery sometimes focus on a claimed lack of harm rather than the risks the patient faced by having the surgery. In other words, when the patient gambles (by having surgery) and there is a bad outcome, the defense is that the patient knew what was at stake. But when the doctor gambles (by recommending and performing an unnecessary surgery), the argument may morph into one that claims the risk (of the bet) was small, and there was not that much potential harm at stake. There are always risks with surgery, however, and this is especially true with any significant degree of anesthesia for surgery. Death, stroke, paralysis, bleeding, infection, are just some of the risks the patient may face, not to mention the costs associated with the procedure. Unnecessary surgeries are harmful for all these reasons even in patients who do not wind up severely injured or dead as a result.
Why are Unnecessary Surgeries Performed?
Surgeons themselves have stated 2 primary reasons that unneeded surgeries continue to be performed:
"1. We perform surgery because we have been trained to do so and because 'we have always done it this way' or we simply do not know any better‚ [and]
2. We are incentivized to perform surgical procedures, either for financial gain, renown, or both."7
To understand both of these personal incentives for the surgeon, they should be considered separately.
Financial Incentives

By virtue of the opioid epidemic, the public is well aware that healthcare fraud occurs and is a problem for our country. The last decade has witnessed many headlines of lawsuit allegations, investigations, guilty pleas, or convictions concerning this problem.8 There are a number of reasons that drive medical overtreatment in the United States, and the degree of the problem varies by geographic region.9 Physicians' financial interests in our U.S. fee-for-service model are only a part of the problem. A profit-driven surgeon agenda is likewise a problem, since over 70% of U.S. doctors themselves believe that other doctors "are more likely to perform unnecessary procedures when they profit from them."10 Some doctors acknowledge the inherent conflict of interest that occurs because surgeons "are paid approximately ten times more money to perform surgery than to manage your problem conservatively."11 So, financial pressures can lead to unnecessary surgery. As one doctor quotes his residency professor, "[t]here is nothing more dangerous than a surgeon with an open operating room and a mortgage to pay."12
In addition to these factors, some surgeons have consulting or speaking agreements with medical device manufacturers, and it has been pointed out that "[s]ometimes the same doctors have performed a record number of implants for that company."13 In addition to surgeons receiving consultant fees, such agreements often result in payments to them for trips, travel, lodging, food, honoraria, gifts, continuing education, etc.14 The potential for a conflict of interest in this setting can thus lead to a surgeon using a particular type of surgical device, even when it is not the right one for the patient. As one advocate against profit-driven health care has suggested, "[y]ou kind of don't want your surgeon to be in bed with the device industry."15
There is a known "symbiotic" relationship between medical device manufacturers and many surgeons, in that surgeons often contribute work and intellectual capital to a device-maker which, in turn, provides those surgeons with an important source of revenue.16 However, problems arise when surgeons don't disclose those potential conflicts in studies they publish about a device17 or, even worse, when surgeons decide to perform a given surgery due to their relationship with the device manufacturer instead on what is in the patient's best interests. Some device-makers have even paid millions of dollars to settle cases involving allegations of improper payments to surgeons.18
Additionally, the potential conflicts of interest noted above don't end with the surgeon. Many teaching hospitals have come under scrutiny for accepting from medical device manufacturers the types of revenue noted above.19 Also, many surgeons are owners or co-owners of ambulatory surgical centers. While doctor-ownership of surgery centers is permissible,20 and can arguably provide more focused or flexible procedures for many patients,21 this ownership model has also been reported to create conflicts of interest, sometimes affecting surgical decisions and leading to a higher volume of surgeries.22 It should also be noted that private insurers and/or the Centers for Medicare and Medicaid Services (CMS), pay surgeons more for certain types of surgeries when they are done through "open" (full) surgical means rather than minimally invasive surgery (laparoscopy), even though the less invasive operation may be safer.23 This practice is another financial incentive for surgeons to perform more extensive surgery than is necessary, even when these types of surgeries are medically justified.
Professional Incentives
There are also professional incentives that have the potential to drive surgeons toward unnecessary procedures. This can include situations where hospital administrators put pressure on surgeons to generate more money by performing more procedures,24 or where hospitals or hospital systems have purchased very expensive surgical equipment or devices and need to justify their use. Likewise, in order for surgeons to be able to perform newer or more technically complex surgical procedures, their hospitals may often require that they perform a minimum number of these procedures every year or two years. The minimum case-volume of such procedures may be imposed by a surgeon's hospital to demonstrate ongoing competence in the procedure, since non-use of these operations can affect how well they are performed.

The American College of Surgeons, for example, notes that "[f]or some complex procedures, published evidence suggests that a high case volume is associated with improved surgical outcomes."25 This is because surgical skills in performing various procedures are subject to decay.26 So, for surgeons to continue to receive professional privileges at a hospital (reappointment or re-credentialing) to perform these procedures, they may have to meet an annual or bi-annual quota of them.27 The surgeons need to not lose these skills, and the need to be able to continue to perform the procedure in a hospital, can therefore be another professional incentive why a surgeon may be motivated to perform a certain surgery more often or frequently than it is required.
Contact Us
The lawyer who is experienced in handling unnecessary surgery cases will know and understand these subjects and the important aspects of the surgery and medical information. He or she will be able to work with qualified expert witnesses in surgery and surgical subspecialties to determine and prove how and why it occurred, and how it should have been prevented. The attorneys at Clore Law Group have significant experience and expertise with handling unnecessary surgery error cases to successful resolution. If you or a loved one experienced a surgical error and harm, you can email us at [email protected], or call us Toll-Free at 1-800-610-2546 for a free and confidential consultation.
Sources
- Stahel PF, Why do surgeons continue to perform unnecessary surgery?, Vol. 11, No.1, Pat Safety in Surg., pp. s13037-0117-6 (2017). at: https://pssjournal.biomedcentral.com/articles/10.1186/s13037-016-0117-6.
- Id.
- Id. See Lyu Xu T, et al, Overtreatment in the United States, PLOS One (Sep. 6, 2017), pp. 4-5, at: https://doi.org/10.1371/journal.pone.0181970; Eisler P, Hansen B, Doctors perform thousands of unnecessary surgeries, Jun. 19, 2013 (pointing out that since the 1970's, "things haven't changed very much" according to Dr. Lucian Leape), accessible online at: https://www.usatoday.com/story/news/nation/2013/06/18/unnecessary-surgery-usa-today-investigation/2435009/; Editor, Do You Need That Surgery? How To Decide, And How To Pick A Surgeon If You Do, Jul 19, 2019, pp.4-5 (quoting Dr. Marty Makary, pancreatic surgeon at Johns Hopkins: "[u]nnecessary surgeries happen all the time...If there's one theme in the medical literature in the past five years, it's that we've been overdoing it". (pp. 4-5)). See also Burke AB, Gilmore S, et al, A Dose of Insight, Surgery Risks: Through the Lens of Malpractice Claims, p. 7 (Coverys Feb. 2020), at: https://coverys.com/PDFs/Coverys-A-Dose-of-Insight-Surgery-Risks.asp
- Stahel, Why do surgeons continue to perform unnecessary surgery?, fn.1 above. Also note that a surgery may be necessary only for an unnecessary reasons such as a misdiagnosis; whereas, with a correct diagnosis an operation would not be necessary. See, e.g., Tosczak M, Errant Cancer Diagnosis, Unneeded Surgery Leaves North Wilkesboro Woman with Pain, Numbness, May 21, 2018, at: https://www.northcarolinahealthnews.org/2018/05/21/22624/.
- Eisler P, Doctors perform thousands of unnecessary surgeries, fn.3 above; Barron J, Unnecessary Surgery, The New York Times, Apr. 16, 1989, at: https://www.nytimes.com/1989/04/16/magazine/unnecessary-surgery.html; Hospice International staff, Research Finds Vast Majority of Tonsillectomies are Unnecessary, HospiMedica Daily Clinical News, Dec. 6, 2018, at: https://www.hospimedica.com/research-finds-vast-majority-of-tonsillectomies-are-unnecessary/articles/294776017/research-finds-vast-majority-of-tonsillectomies-are-unnecessary.html; and Epstein NE, Hood DC, 'Unnecessary' spinal surgery: A prospective 1-year study of one surgeon's experience, Vol. 2, No. 83, Surg Neurol Int. (2011).
- Eisler P, Doctors perform thousands of unnecessary surgeries, and Lyu Xu T, Overtreatment in the United States, both in fn.3 above.
- Stahel, Why do surgeons continue to perform unnecessary surgery?, fn.1 above.
- Associated Press, Feds: South Dakota Doc Made Millions on Unneeded Surgeries, Nov. 14, 2019, at: https://www.usnews.com/news/us/articles/2019-11-14/feds-south-dakota-doc-made-millions-on-unneeded-surgeries; Associated Press, Jury Convicts Doctor of Scheme to Perform Unnecessary Surgeries on Women, at: https://www.justice.gov/usao-edva/pr/jury-convicts-doctor-scheme-perform-unnecessary-surgeries-women; Koleva G, Largest U.S. Hospital Chain Probed for Medically Unnecessary Heart Procedures, Aug. 6, 2012, at: https://www.forbes.com/sites/gerganakoleva/2012/08/06/largest-u-s-hospital-chain-probed-for-medically-unnecessary-heart-procedures/#2fc07caf53fe; CBS 4 News Staff, McAllen doctor convicted of healthcare fraud, aggravated identify theft, Nov. 22, 2015, at: https://valleycentral.com/news/local/mcallen-doctor-convicted-of-healthcare-fraud-aggravated-identity-theft; Garcia B, Zamora Quezada convicted of multiple counts of healthcare fraud; wife acquitted, Jan. 15, 2020; and U.S. DOJ, Office of Public Affairs, Release, Oct. 28, 2019, Sanford Health Entities to Pay $20.25 Million to Settle False Claims Act Allegation Regarding Kickbacks and Unnecessary Spinal Surgeries, at: https://www.justice.gov/opa/pr/sanford-health-entities-pay-2025-million-settle-false-claims-act-allegations-regarding.
- See, e.g., Eisler P, Doctors perform thousands of unnecessary surgeries, fn.3 above; Barron J, Unnecessary Surgery, fn.5 above.
- Lyu Xu T, Overtreatment in the United States, fn.3 above, at pp. 1, 8.
- Crouch M, 45 Secrets Surgeons Won’t Tell You, The Healthy, Nov. 25, 2019, Updated Nov. 14, 2020, at Secret: Practically all surgeons have an inherent financial conflict of interest (quoting Dr. James Rickert, orthopedic surgeon in Indiana, who also says that “the field of orthopedics ‘is one of the worst offenders’”). See Clark C, Medpage Today, Orthopedists’ Financial Conflicts Can Hurt Patients, Surgeon Says, Mar. 22, 2015, p. 1, at: https://www.medpagetoday.com/surgery/orthopedics/50601.
- Id. at Secret: Always ask about nonsurgical options and whether there's anything wrong with waiting a little while (quoting Dr. Jones).
- Id. at Secret: Some orthopedic surgeons make millions in soft consulting agreements with device manufacturers (quoting Dr. Marty Makary).
- Cox, CE, Physician Conflict of Interest Disclosures to Journals for Device Industry Ties Falls Short, tct/md the heart beat, Aug. 24, 2018, p. 2, at: https://www.tctmd.com/news/physician-conflict-interest-disclosures-journals-device-industry-ties-fall-short.
- Editor, Do You Need That Surgery?, fn.3 above (quoting Shannon Brownlee, Senior VP of the Lown Institute, https://lowninstitute.org/lown-issues/accountability/). Financial relationships between medical device vendors and surgeons have also been noted to lead to improper surgical implants, see, e.g., Crouch M, 45 Secrets Surgeons Won't Tell You, fn.11 above, Secret: If you need a medical device, ask if your doctor has a financial relationship with the vendor (quoting Dr. James Rickert, "if so, chances are you're going to get that type of joint or screw, even if it's more expensive or not the most appropriate.").
- Cox, CE, Physician Conflict of Interest Disclosures, fn.14 above, at p. 2.
- See, e.g., Wolters Kluwer Health, Financial conflicts of interest are often not disclosed in spinal surgery journals, at: https://medicalxpress.com/news/2020-07-financial-conflicts-disclosed-spinal-surgery.html.
- See, e.g., U.S. Attorney's Office, Dist. of NJ Release, Medical Device Maker to Pay $18 Million to Settle Allegations of Improper Payments to Physicians, Oct. 14, 2020, at: https://www.justice.gov/usao-nj/pr/medical-device-maker-pay-18-million-settle-allegations-improper-payments-physicians, and U.S. Dep't of Justice (DOJ), Public Affairs, Medtronic to Pay Over $9.2 Million to Settle Allegations of Improper Payments to South Dakota Neurosurgeon, Oct. 29, 2020, at: https://www.justice.gov/opa/pr/medtronic-pay-over-92-million-settle-allegations-improper-payments-south-dakota-neurosurgeon.
- Adams, K, Drug, device companies' payments to teaching hospitals may spark conflict of interest, study suggests, Becker's Hospital Review, Sep. 9, 2020.
- Although there are various limitations on physician self-referrals of patients to various facilities in which they have an ownership, see Stark Act, 42 U.S.C. sec. 1395nn (allowing the U.S. Dep't of Health and Human Services to pursue civil penalties for violations), this law does not apply to ambulatory surgical facilities. The federal anti-kickback (criminal) statute does, however, apply to ambulatory surgical and other facilities. It prohibits any person from knowingly and willfully providing (soliciting, paying, offering, or accepting) remuneration to induce, or in exchange for, referrals. 42 U.S.C. sec. 1395a-7b(b). Further, the federal false claims act presents a person from defrauding the federal government by presenting a fraudulent claim for payment. Violations can result in a judgment against the defendant for up to 3 times the amount of damages of suffered by the U.S. Treasury because of the fraud, plus civil fines. 31 U.S.C. secs. 3279-3733. This has led to civil whistleblower (qui tam) cases against healthcare providers/entities for such violations, including for allowing ongoing unnecessary surgeries. See U.S. DOJ, Office of Public Affairs, Release, Sanford Health Entities to Pay $20.25 Million to Settle False Claims Act Allegation Regarding Kickbacks and Unnecessary Spinal Surgeries, Oct. 28, 2019, at: https://www.justice.gov/opa/pr/sanford-health-entities-pay-2025-million-settle-false-claims-act-allegations-regarding. You can look search the CMS database for payments made by medical device and drug companies to physicians and teaching hospitals, at: https://openpaymentsdata.cms.gov/. Another online source for this type of information can be found at: https://projects.propublica.org/docdollars/.
- See, e.g., Badlani N, Ambulatory Surgery Center Ownership Models, Vol. 5 (Supp. 2), J Spine Surg., pp. S195-S203 (Apr. 12, 2019), available at: http://jss.amegroups.com/article/view/4543/pdf; the American Medical Association (AMA)-Advocacy Resource Center, Defending Physician Ownership‚ Legislative Talking Points Defending Free-Standing ASCs (Jan. 2015 Physician Ownership Whitepaper), at: https://aaos.org/globalassets/advocacy/state-advocacy/specialty-hospitals/defending-physician-ownership.pdf; and Advancing Surgical Care (ASC), Benefits of Physician Ownership, at: https://www.ascassociation.org/advancingsurgicalcare/asc/benefitsofphysicianownership.
- See, e.g., Peeples L, Financial incentives affect surgical decisions, Health News, Aug. 18, 2010, available at: https://www.reuters.com/article/us-financial-incentives-idUSTRE67H4NH20100818; Hollingsworth JM, Ye Z, et al, Physician-Ownership of Ambulatory Surgery Centers Linked to Higher Volume of Surgeries, Vol. 29, No. 4, Health IT: The Road to 'Meaningful Use,' HealthAffairs, at: https://www.healthaffairs.org/doi/10.1377/hlthaff.2008.0567; Strope AS, Daignault S, et al, Physician ownership of ambulatory surgery centers and practice patterns for urological surgery: Evidence from the State of Florida, Vol. 47, No. 4, Med Care. pp. 403-410 (Apr. 2009).
- See, e.g., Fader AN, Xu T, et al, A perverse quality incentive in surgery: implications of reimbursing surgeons less for doing laparoscopic surgery, Vol. 30, No. 11, Surg Endosc. pp. 4665-4667 (Nov. 2016), accessible at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5576022/pdf/nihms887003.pdf.
- Crouch M, 45 Secrets Surgeons Won't Tell You, fn.11 above (quoting Dr. Marty Makary: "This is not an insurance company putting pressure on doctors; this is not a government regulation. This is private hospitals pushing doctors to generate more money by doing more procedures. It goes on at America's top hospitals. The Cleveland Clinic has said this system of paying doctors is so ethically immoral that it started paying its doctors a salary no matter how many operations they do.").
- American College of Surgeons, Statement on Credentialing and Privileging and Volume Performance Issues, Apr. 1, 2018, p. 2, at: https://www.facs.org/about-acs/statements/111-credentialing.
- See Perez RS, Skinner A, et al, Prevention of Surgical Decay, Vol. 178, No. 10, p. 76 (2013); Cecilio-Fernandes D, Cnossen F, et al, Avoiding Surgical Skill Decay: A Systematic Review on the Spacing of Training Sessions, Vol. 75, No. 2, J Surg Educ. pp. 471-480 (Mar-Apr. 2018), at: https://www.sciencedirect.com/science/article/abs/pii/S1931720417300442; and Arthur W, Jr., Bennett W, Jr., et al, Factors that Influence Skill Decay and Retention: A Quantitative Review and Analysis (Nov. 13, 2009), at: https://www.tandfonline.com/doi/abs/10.1207/s15327043hup1101_3.
- See Wlazelek A, LVH Sets Heart Surgery Quota System, Doctors Say Action Emphasizes Quantity Over Quality, The Morning Call (Mar. 27, 1994), at: https://www.mcall.com/news/mc-xpm-1994-03-27-2956460-story.html.