Cerebral Palsy: When is it Due to Childbirth Malpractice?

What is Cerebral Palsy?
Cerebral palsy (CP) is a medical disorder that affects a child's ability to move, or control his or her muscles or posture, that occurs from damage to the developing brain. CP is the most common motor disability in children, affecting around 1/323 children according to the CDC.1 CP can result from certain conditions while the baby is in the mother's womb, i.e. congenital, or from some injury during labor or at birth, i.e. acquired.2 Signs of the disorder (CP) in infants and toddlers include delays in movement milestones, such as in rolling over, sitting, standing, or walking. CP can usually be diagnosed by 2-3 years of age.3
When Can it be Due to Medical Malpractice at Childbirth?
When CP occurs due to events in labor or delivery of a baby, it is often from a lack of oxygen and/or trauma to the brain. When the body is deprived of oxygen, this is known as asphyxia. While brief periods of poor oxygen supply or interrupted breathing are common for the fetus in labor and at delivery, there are a number of events that can occur in labor or delivery that, if not timely corrected, can result in lengthy periods of oxygen deprivation that can damage the fetus' brain from asphyxia. According to estimates, about 15-20% of the time CP occurs due to some asphyxial damage to the baby's (fetal) brain that occurs while the mother is in labor or childbirth, which is known as the "perinatal" or "intrapartum" period.4 Significant trauma to the fetus' head during labor or at delivery can also cause brain injury resulting in CP.5 All of these situations can amount to medical malpractice or negligence.
Asphyxia
Severe conditions in labor such as placental abruption, uterine rupture, umbilical cord accidents, maternal seizures, profound maternal hypotension (low blood pressure), etc., can cause asphyxial episodes to the fetus if immediate or emergency delivery does not occur. Likewise, abnormal fetal position, prolonged labor with pushing, and/or conditions such as the mother having excessively long or strong contractions, or a very high maternal fever, can result in asphyxial changes or contribute to brain injury from asphyxia if these things are not timely and properly corrected, or the baby is not promptly delivered.6  Sometimes these conditions are immediately apparent, and the failure to effect an immediate or emergency delivery of the baby may constitute medical malpractice. Other times, one of more of these conditions may be suspected from the electronic fetal monitoring (EFM) of the mother and baby, again requiring action by the nurse or doctor. When any of the foregoing type conditions start to result in asphyxia or problems to the fetus, the EFM of the mother and baby will show fetal heart rate pattern decelerations and/or diminishment from normal variation in heart beats. This is what should alert obstetrical nurses and obstetricians to the need for measures to correct the asphyxia or for urgent delivery of the baby. The failure to timely recognize these EFM changes, or to timely intervene when they are present on the monitor, can constitute negligence by the nurse or doctor, and thus medical malpractice.
Sometimes these conditions are immediately apparent, and the failure to effect an immediate or emergency delivery of the baby may constitute medical malpractice. Other times, one of more of these conditions may be suspected from the electronic fetal monitoring (EFM) of the mother and baby, again requiring action by the nurse or doctor. When any of the foregoing type conditions start to result in asphyxia or problems to the fetus, the EFM of the mother and baby will show fetal heart rate pattern decelerations and/or diminishment from normal variation in heart beats. This is what should alert obstetrical nurses and obstetricians to the need for measures to correct the asphyxia or for urgent delivery of the baby. The failure to timely recognize these EFM changes, or to timely intervene when they are present on the monitor, can constitute negligence by the nurse or doctor, and thus medical malpractice.
Trauma
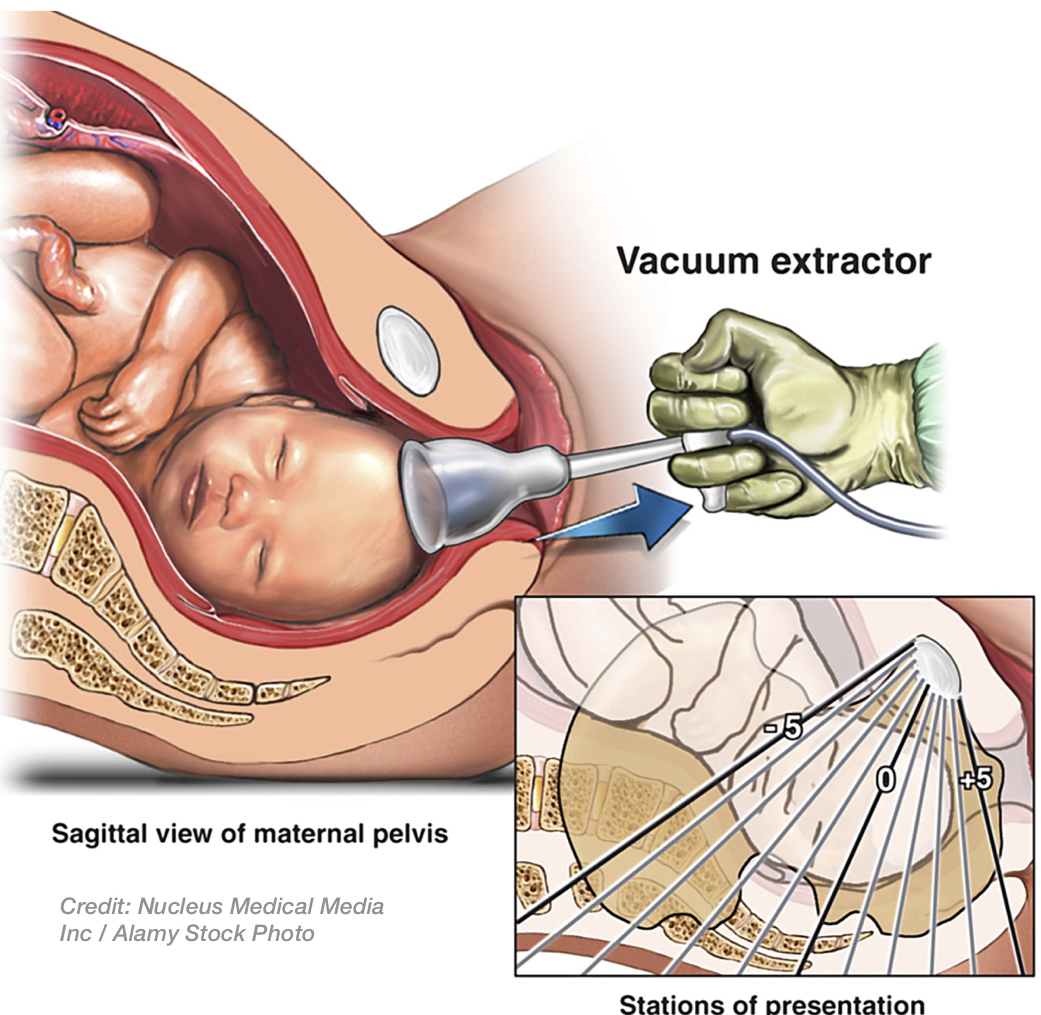
Excessive compression to the fetus' head can occur while it is in the birth canal, from overly strong maternal contractions, and this can also result in traumatic injury and/or asphyxia to the fetal brain--especially if the fetal head is in the wrong position and/or the labor-inducing drug Pitocin is being given to the mother. Trauma to the fetal head can also happen during delivery, when instruments like forceps or vacuum extractors are improperly used by the doctor or the midwife, including if the fetus is too high in the birth canal (i.e. high fetal station). Physical trauma can cause direct injury and bleeding to the brain, and may worsen the asphyxia in the brain.
What is HIE?
As a result of either asphyxial events or trauma, the baby can experience a birth injury. Specifically, the baby's birth injury may be a type of brain condition called "hypoxic-ischemic encephalopathy" (HIE). HIE simply means that there was a lack of oxygen supply to the brain and organs (hypoxia), and/or low or restricted blood flow (ischemia) to the fetus that resulted in a brain disorder (encephalopathy). HIE is a significant cause of infant impairment and mortality.
What are Signs or Symptoms of HIE?
If HIE is due to events in labor or delivery, the baby will often have seizures soon after birth, and radiology imaging, particularly neuroimaging such as CT and MRI hours-to-days later, may show areas of swelling, damage, and/or patterns of damage, in the baby's brain that can be linked to the events in labor or delivery. The type and location of this brain damage often depends on the degree and length of the asphyxia, or trauma, that occurred. With severe sudden or acute intrapartum asphyxial events, for instance, the baby may have brain injury in certain parts of the brain, while with partial or prolonged asphyxia, different areas of the brain may be injured. Oftentimes, the baby may have damage seen on MRI that reflects both, i.e. a mixed pattern of severe and prolonged asphyxia. Additionally, HIE due to asphyxia results in some amount birth depression (i.e. lower birth Apgar Scores--measurements of heart rate, muscle tone, breathing, skin color, etc.), and, depending on the cause and timing, biochemical changes such as excessive acid in the blood may be, but are not always, seen with laboratory testing just after birth (i.e. low pH, negative base excess); also, dysfunction may be revealed in other organs besides the baby's brain.7 So, to reiterate, these are signs or symptoms of HIE that may be seen in the baby:
At Birth:
- Low Heart Rate
- Poor Muscle Tone
- Weak or No Breathing
- Pale or Bluish Skin Color
After Birth:
- Excessive Acid in the Cord Blood
- Seizures or Seizure-Like Activity
- Other Organ Dysfunction (e.g. kidney, liver, lungs or heart, etc.)
- Neuroimaging (CT/MRI) Evidence of Swelling and Damage
HIE Can Result in CP
The brain injury from HIE can result in a child developing CP8. Yet, the baby with HIE does not always develop severe, permanent brain injury or CP. If the baby is treated shortly after birth with proper medications, ventilation, and hypothermia (cooling the baby's brain/body), sometimes it can prevent mild or moderate permanent damage. Many times, however, the HIE brain damage is permanent, and the baby may have severe, life-long intellectual or mental (cognitive) damage, blindness, deafness, epilepsy, and/or other neurological problems in addition to CP. When there is significant injury, a type of CP often ensues where the baby will have involuntary movements of the extremities, such as spastic quadriplegia, or an athetoid or dyskinetic type of CP.
The Lawyer's Role
We are well-versed in handling HIE/CP cases, and familiar with the important medical literature about HIE, CP and their causes, as well as the factors and evidence that are important to assess. We work with highly qualified physicians and expert witnesses, in numerous fields, to ascertain whether and why a given child's HIE/CP was due to medical malpractice from events prior to or during labor and/or delivery. And we have had significant past success in prosecuting these types of cases to substantial settlements and jury trial verdicts.
Contact Us
If you are concerned that your child or a loved one's may have HIE or cerebral palsy due to events in labor or delivery, or due to medical malpractice events that occurred in a healthcare setting, you can email us at [email protected], or call us Toll-Free at 1-800-610-2546 for a free and confidential consultation.
Sources
- Centers for Disease Control and Prevention (CDC), Data & Statistics for Cerebral Palsy, which can be found at: https://www.cdc.gov/ncbddd/cp/data.html.
- Id. at Causes and Risk Factors: https://www.cdc.gov/ncbddd/cp/diagnosis.html.
- CDC, Screening & Diagnosis of Cerebral Palsy: https://www.cdc.gov/ncbddd/cp/diagnosis.html; see also Robertson, CM & Perlman, MB, Follow-up of the term infant after hypoxic-ischemic encephalopathy, Paediatr Child Health, Vol 11, No. 5, pp. 278-282 (May-June 2006).
- Jassien, JM & Johnston, MV, Perinatal hypoxic-ischemic encephalopathy, Neurol Link (1994, update 6/12/17), at: http://www.medlink.com/article/perinatal_hypoxic-ischemic _encephalopathy. See also Edwards, AD, Patel, J, et al, Prevention of acquired neurological impairment in the perinatal period, Vol 63, Supp. 1, BMJ of Neurol, Neurosurg & Psych., p. 8 (1997)(estimating an incidence of 10% – 30% in developed countries).
- National Institute of Neurological Disorders and Stroke (NINDS), National Institute of Health (NIH), Cerebral Palsy–Hope Through Research, p. 7, at: http://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Cerebral-Palsy-Hope-Through-Research.
- NINDS/NIH, n5, at 6-7.
- American College of Obstetricians & Gynecologists, Executive Summary: Neonatal Encephalopathy and Neurological Outcome, Vol 123, No. 4, pp. 896-901 (2d ed. 2014); see also Hermansen, MC, The acidosis paradox: asphyxial brain injury without coincident acidemia, Develop Med & Child Neurol., Vol 45, pp. 353-56 (2003); Robertson, n3, at 277-80.
- See, e.g., Robertson, n3, at 278-80; NINDS/NIH, n5, at 6-7.