Cancer Misdiagnosis & Mistreatment
Descriptions of cancer can be traced back to the ancient Egyptians, some of whose mummified remains contained the earliest evidence of cancer in humans. In fact, surgery to remove breast cancer in Egyptian women was performed with cauterization around 3000 BC. Famous Greek and Roman physicians are responsible for today's basic cancer terminology, since they termed the disease "carcinoma," to refer to the crab-like and tentacle appearance of tumors (Hippocrates, 460-370 BC), and thus "cancer" (Celsus, 50-28 BC), as well as "sarcoma" to refer to cancer having a fleshy or raw-meat appearance (Galen 200-130 BC). The latter physician, Galen, also described the swelling associated with cancerous tumors as "oncos", from which "oncology," the field of cancer medicine, is derived.1
What is Cancer?
The term "cancer" encompasses diseases in which there is uncontrolled division of abnormal cells in the body that invade the organ from which it originates, and that has the potential to spread to other parts of the body through the blood or the lymphatic system.2
What are the Types or Classifications of Cancer?
The main types of cancer are categorized depending on where they originate:
- "carcinomas" begin in the tissues or skin that line organs;
- "sarcomas" start in bone, fat, connective tissue, cartilage, blood vessels, etc.;
- "leukemias" begin in the blood-forming organs or tissue such as the bone marrow;
- "lymphomas"originate in the immune (lymphatic) system;
- "myelomas" start in the bone marrow, and share many features of lymphoma; and,
- "central nervous system cancers" begin in the brain or spinal cord.3
Cancers are further classified in one of two ways, either by the body organ or location where the primary cancer originated, and/or by the way the cancer tissue structures and cells look under a microscope, which is known as "histology"—part of the medical field of pathology. So for example, to differentiate a certain type of primary lung cancer tumor from other lung cancers, a medical diagnosis of "squamous cell lung carcinoma," would mean a specific histologic type of cells (squamous cells) that line the bronchial airways and are cancerous (lung carcinoma).
How Does Cancer Develop?
We all remember from basic high school biology that cells in our body are in a continual cycle of growth, division, and death, as regulated by instructions from our DNA. We may recall that mitosis refers to cell division, where one cell divides to become two identical cells, and so 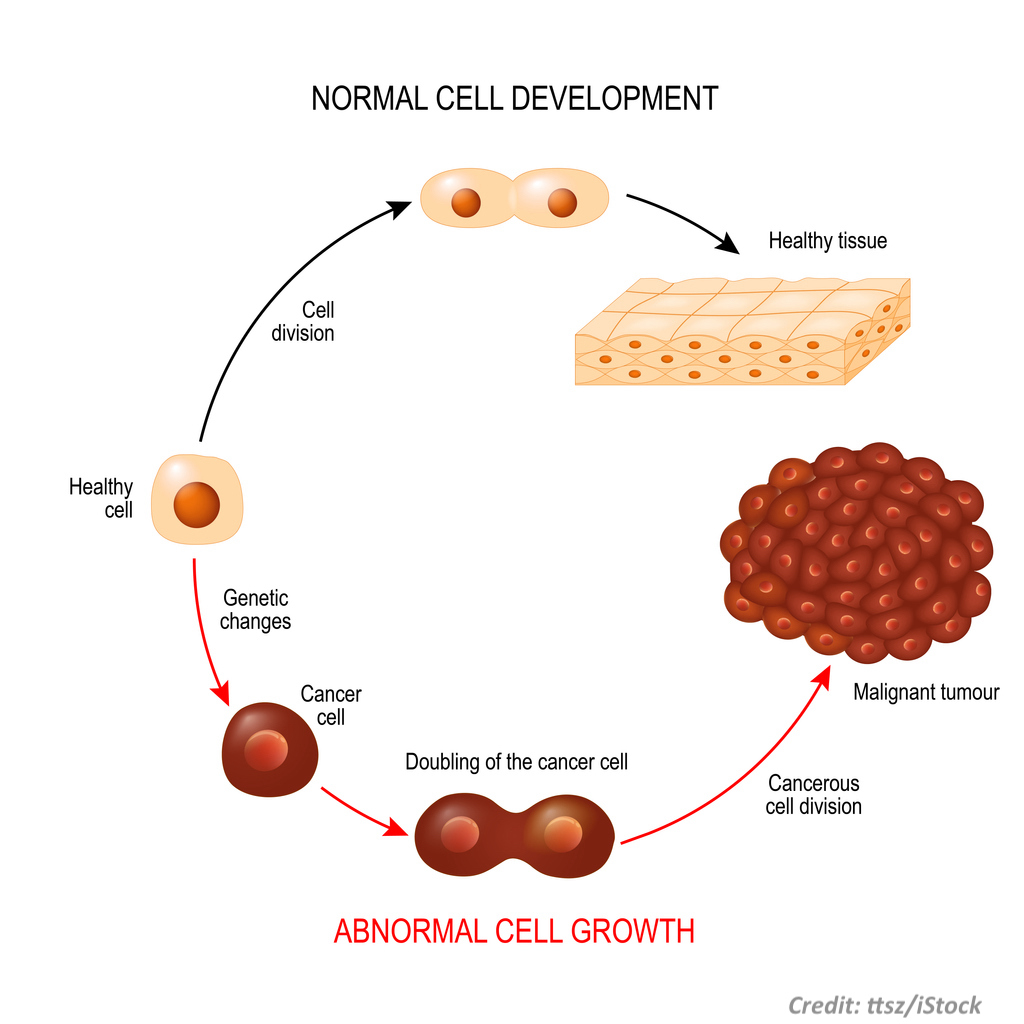 on and so forth. Normal cells can change though, before and after mitosis, to become abnormal. These mutations can happen for various reasons, due to genetics, viruses, carcinogens, etc. There are phases in these abnormal changes, and cancer may or may not arise as a result. For instance, abnormal cell tissue may become hyperplastic, where there is an increased rate of reproduction of normal cells, and this may then progress to dysplasia, where there is abnormal cell growth seen under a microscope. These conditions are often called "precancerous" tumors, masses, or lesions. The body's immune system naturally fights against this progression, and cells die as a result, as well due to normal cell DNA instructions for cell death (apoptosis).4
on and so forth. Normal cells can change though, before and after mitosis, to become abnormal. These mutations can happen for various reasons, due to genetics, viruses, carcinogens, etc. There are phases in these abnormal changes, and cancer may or may not arise as a result. For instance, abnormal cell tissue may become hyperplastic, where there is an increased rate of reproduction of normal cells, and this may then progress to dysplasia, where there is abnormal cell growth seen under a microscope. These conditions are often called "precancerous" tumors, masses, or lesions. The body's immune system naturally fights against this progression, and cells die as a result, as well due to normal cell DNA instructions for cell death (apoptosis).4
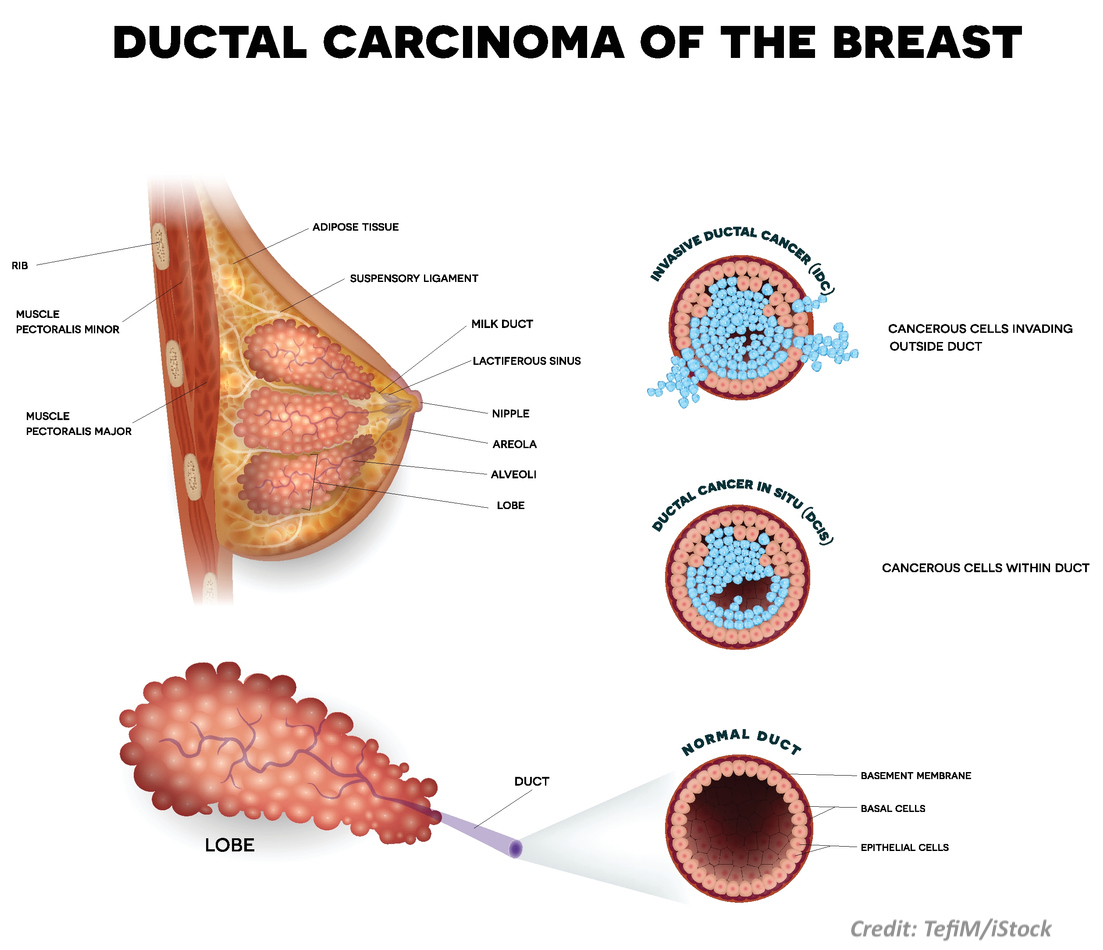
When a tumor with cancer-looking cells develops and is still located at the site of where it originated, without having invaded the organ where it first formed, it is referred to as "in situ." Yet when the cancerous tumor cells spread to and invade the organ where it began, it is is considered "invasive" cancer. An example of this can be seen in the illustration to the right, of breast cancer that formed first in a duct of the breast, i.e. ductal, that is at first "in situ" (a precursor to cancer)but then continues over time to become invasive in that organ.5
How Does Cancer Continue to Grow & Spread?
Cancerous tumors need sustenance in order to continue to survive, replicate, and grow. This means they need to develop their own blood supply. The process, which occurs when cancer tumors give off chemical signals to stimulate new blood vessels to grow from preexisting ones, is known as "angiogenesis."6

Angiogenesis occurs to support cancer growth, and is necessary for cancer spread to regional or distant locations in the body, which is known as cancer "metastasis."7 Further, in order for a metastatic cancer to survive and repeat the replication and growth process, it also needs angiogenesis. All throughout this process, the body's immune system continues to fight and kill cancer cells but with a metastasis (or metastases, plural) some of the cancerous cells may still reach nearby lymph node(s) or distant organ(s) and continue their uncontrolled cancer growth.
Why is Cancer Screening and Early Detection Important?
Many cancers are highly curable or treatable when they are removed or destroyed early. This is why early detection is so important. If cancer-looking cells are diagnosed when the tumor is in situ, or before invasive cancerhas grown large enough to permit significant spread or metastasis, the rates of complete cure, not just remission, can be very high after treatment. Conversely, depending on the type of cancer and its location, the rates of cure and length of cancer-free survival time may be much worse or lower if significant cancer growth/invasion or metastasis has already occurred due to a delay in detecting or diagnosing, and/or properly treating it.
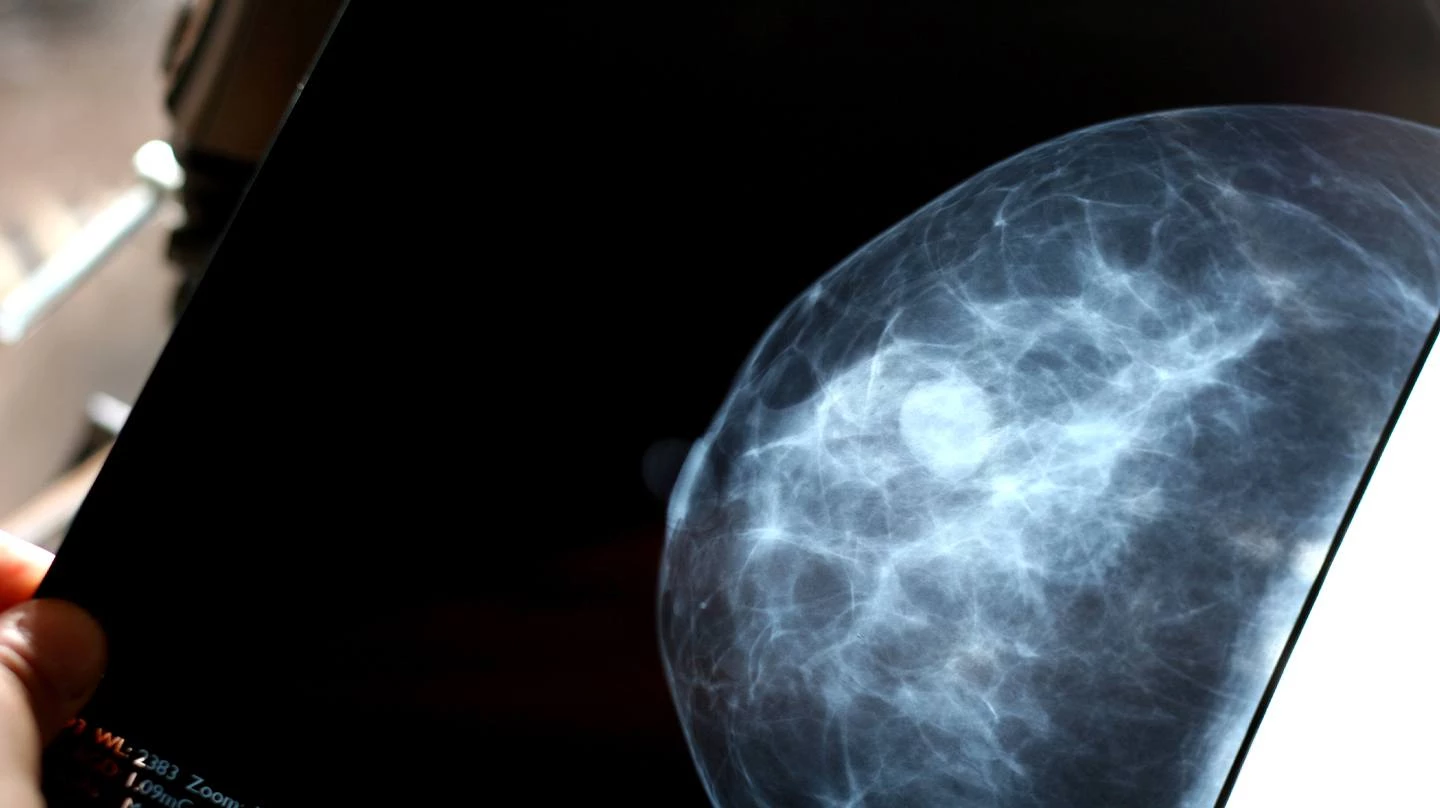
The screening recommendations that doctors use for cancer depend in part on patient risk of developing a certain type of cancer. However, there are certain universal or uniform recommendations for periodic cancer screening, for: breast cancer (with mammogram) and cervical cancer (with pap smear) in women; for lung cancer (with low-dose CT) in smokers; and, for colorectal cancer (with colonoscopy/stool tests) cancer screening in adults aged 50-75. In general, screening recommendations are universally recommended when medical studies show the benefits outweigh the harms, and that the screening is effective at detecting cancer when it can still be cured.8
What is the Staging System for Cancer?
The American Joint Committee on Cancer (AJCC) is the official organization in the United States that provides the staging systems that defines how advanced a cancer is, and that is used to guide surgeons, pathologists, radiologists, oncologists, and other health care providers in diagnostic and treatment decisions or recommendations. For instance, optimal treatment for cancers detected and diagnosed early may only be surgery or radiation to remove or kill the primary tumor, while multiple drugs (chemotherapy), targeted drug therapy, and/or immunotherapy may be optimal treatment when cancer is not caught until it reaches a more advanced stage.
Although there are different types of staging systems for various types of cancers, the AJCC "TNM" staging system is the most well-recognized. In this system, the: "T" stands for the primary cancer tumor size, characteristics, and/or location; "N" stands for node(s), meaning lymph node status--whether the cancer has spread to lymph node(s) and, if so how many, of what size, where they are located, etc.; and, "M" stands for metastasis to other locations in the body, where and to what extent, etc.9
With this TNM system, the AJCC groups cancers into one of five stages, e.g. 0 – IV, with the best prognosis being at stage 0(generally in situ) and the worst prognosis being at stage IV (usually distant metastasis). Yet, there are many factors that affect prognosis in addition to the stage, including a person's age, genetics, and response to treatment, as well as the traits and grade (histologic) of the cancer.10 Medical research and trials are continually being performed and published for these reasons, about certain types and combinations of drugs or therapies, in order to determine which treatments work best and provide the greatest rates of cure or disease-free survival.
How Often is Cancer Misdiagnosed?
Various studies provide estimates about how often cancer is misdiagnosed in the United States; and it has reported, based on discrepancies between patient diagnoses and autopsy diagnoses, that cancer misdiagnoses happens up to 44% of the time.11
Which Cancers are Most Commonly Misdiagnosed?
In general, the cancers which are commonly misdiagnosed as harmless (benign), or overdiagnosed (as cancer when they are not), are not surprisingly those that are among the most common.12 Hence, the more commonly something is diagnosed, the greater potential there is for it also to be misdiagnosed. With that recognition, however, the most frequent incidence of cancer diagnosis depends in large part on which age group, gender, race/ethnicity, and geographical location you consider.
In one U.S. survey of 400 physicians, almost 80% believed that lymphoma is "the most misdiagnosed cancer," and the surveyed doctors regarded the following cancers as some of the most often misdiagnosed after lymphoma: breast, sarcoma, melanoma, central nervous system, lung, prostate, ovarian.13
A more recent study14based on actual NCI SEER Cancer Registry Data reported these cancers as the five that are most commonly misdiagnosed, along with percentage estimates of misdiagnosis:

Why are Cancers Misdiagnosed?
Human error is a fundamental, root cause of misdiagnosis, and there are a variety of factors that often account for diagnostic errors by healthcare providers, including:
- inadequate time expended in patient care
- miscommunication with patients and/or caregivers
- other lack of information or expertise
- lack of coordinated care, including among specialists
- failure to order timely and appropriate tests or screening
- failure to obtain timely specialty consultation(s)
- failure to provide appropriate instructions to the patient
- failure to follow-up timely with the patient or on the patient's test results

Medical Malpractice Cases for Cancer Misdiagnosis
As discussed in other Insights, in many or most states to prevail on a medical malpractice case, testimony or proof from expert witness(es) is basically required for the patient's attorney to show two things: (1) that there was substandard or improper healthcare amounting to negligence, and (2) that such negligence was more likely than not a cause of the patient's harm or injury (or death).15 With cancer misdiagnosis, and delayed diagnosis, cases, it is this second part, what the law calls "causation," that can sometimes be a challenge. This is because if a misdiagnosis or delay in proper diagnosis occurred for only a very short amount of time, the defense may argue that it likely made no difference in or to the patient's ultimate outcome. In other words, a delay in properly detecting or diagnosing cancer may not have been for long enough to show that, even if cancer treatment had begun earlier when it should have been diagnosed, the patient would likely not have been harmed, injured, or died—meaning that there likely would have been a cure, or that the cancer would likely not have spread, or that much less invasive treatment/therapy would have been required, etc.
Lawyers who successfully handle cancer misdiagnosis cases are mindful of these issues when deciding whether or not to take a case, and in deciding how to try and prove those cases they accept. This process involves obtaining necessary expert testimony from specialists, who may include surgeons, radiologists, oncologists, and/or pathologists for example.Those experts will base their opinions on their knowledge, training, and experience, but they also often rely on pertinent medical literature in their field that deals with cancer growth rates (kinetics), radiology or pathology tumor grading/markers, and staging to show the cancer would likely have been much more treatable or curable if it was diagnosed or detected when it should have been.
In cancer misdiagnosis cases, the victim's body can become a battleground of medical debate. The conflict in evidence usually involves pathology and/or oncology debate about the likely growth rate and time of spread. As mentioned earlier, untreated cancerous cells and their progeny grow and replicate via mitosis (doubling), develop in situ into a tumor or mass if they don't die, later become invasive and over time experience angiogenesis and thus the capacity to spread (metastasize), begin to spread and, if they survive, may seed elsewhere and may replicate, but further angiogenesis is required for the metastasis to survive; otherwise it will remain microscopically dormant.16
The rate at which a primary cancerous tumor grows can sometimes be calculated in malpractice cases by comparing radiology imaging measurements once the tumor was first detected (but not diagnosed as cancer), with measurements on the next or subsequent imaging (and when it is eventually diagnosed). This rate of tumor growth or doubling is known as the "doubling time (DT)." There are various mathematical formulas to calculate the number of doublings that a cancer tumor undergoes from one size to the next, and there are different models to estimate the doubling time (DT) for cancerous tumors.17 Defense attorneys routinely employ the estimated DT defense to claim that the patient's misdiagnosed cancer must have been present for a very long time, and to argue that it must have spread early (when it was microscopic) and before the Defendant's care. There are a number of reasons why these arguments are often wrong or inapplicable to a given medical malpractice case, including because primary cancers don't grow at a constant rate--they grow much more rapidly when they are too small to see, and slow down as they get larger--as well as because metastatic cancers (that occur from spread of the primary) grow much faster typically than the primary (parent) tumors.18
Tumors are three-dimensional objects; so, they double in volume not just circumference. This means, for instance, that a one centimeter (cm) cancerous tumor does not just double once to reach two cm; in actuality, it doubles about 3 times from 1 cm to 2 cm. Since doctors use the metric system in measuring the dimensions of cancer for radiology or pathology purposes, it may help to appreciate tumor doubling sizes as illustrated below. The chart shows a hypothetical lung cancer tumor that is no longer microscopic but is the size of the head of a pencil (about .1 cm or 1 mm) to start with, and then shows the size of that cancer in a certain model as it doubles for a total of 17 times. Note the cancer doubles about 4 times before it reaches about the size of the head of a crayon, and then twice more before it becomes close to the size of a bb. In the illustration, each inverted blue triangle (except the first one) equals one volumetric doubling. So, at 1 cm, the cancer is about the size of a green pea, by 2 cm it is around the size of a cranberry, at 3 cm it is grape-sized, and so forth.
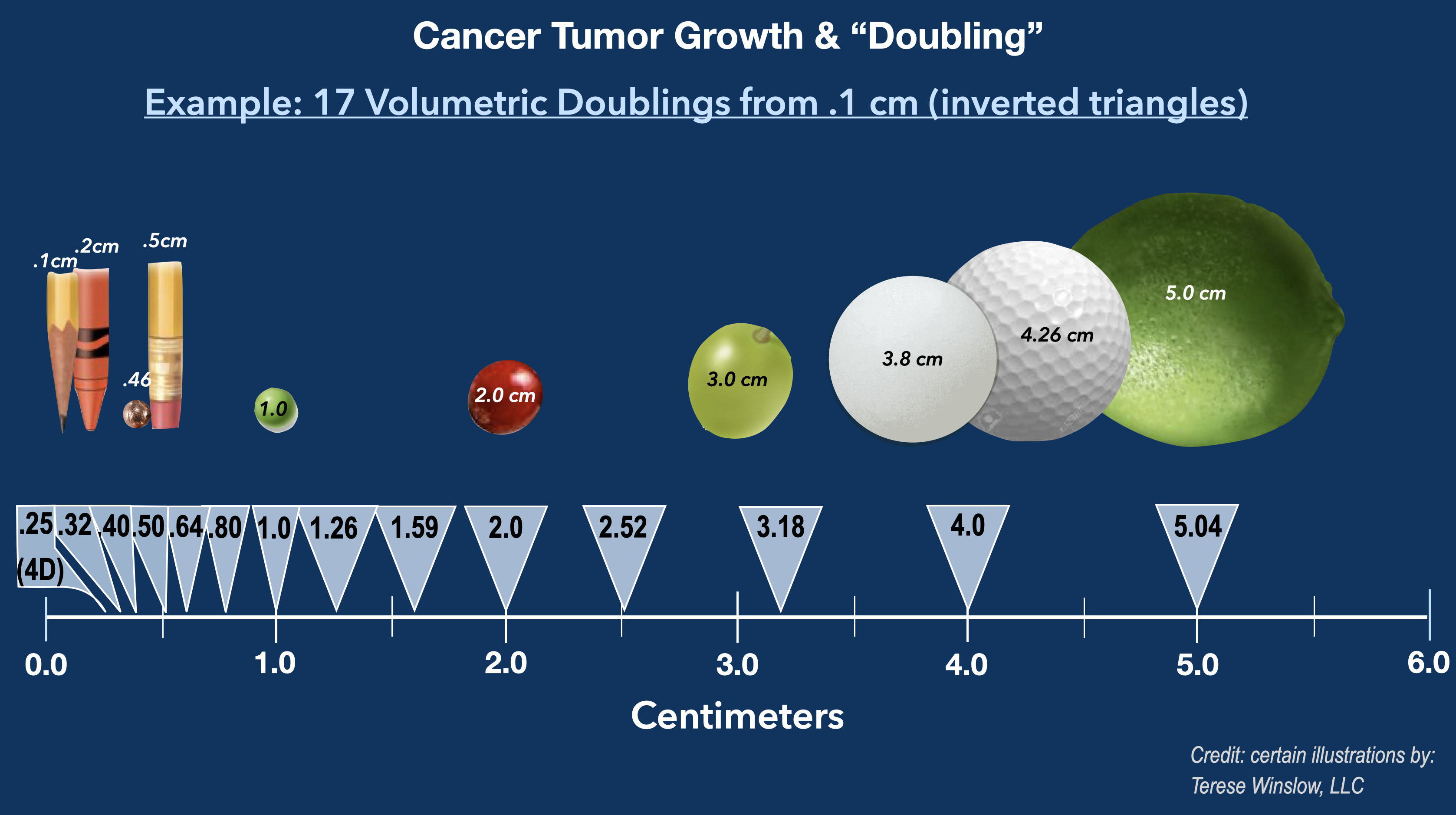
With many solid cancerous tumors, such as of the breast, lung, colon, etc., there are known radiological ranges of DTs published in medical literature, and the factors that account for the speed at which tumors double in volume are those discussed earlier, such as the cancer cell type, grade, genetic factors, etc. If there is adequate time-length between different primary tumor sizes seen on radiology imaging from one point to the next, or on multiple imaging studies over time, then the DT between those points can be ascertained by using a doubling formula (which gives the number of doublings from one size to the next as illustrated above) and dividing by the number of days in between to calculate the DT. Since the size of a primary cancer tumor is a major part of the AJCC TNM staging system, radiological DTs can be used, along with other data, to assist expert witnesses in giving opinions about how the likely treatment and/or outcome (cure rate, disease-free survival) would have been much better had the cancer been diagnosed and treated earlier, when it should have been. DT estimates are not always available or useful in a given case based on the medical facts, however, and as mentioned there are limitations to DT evidence.19 Yet there are also other types of medical test results that patients may have in a given case that can help to prove that earlier and timely diagnosis and treatment would have made a significant difference in their outcome.
When a tumor is misdiagnosed as cancer but it is really not cancer, then of course the concepts of growth kinetics, DT, and staging may be irrelevant. This is because there is not a case of neglect that caused harm due to a delay, but neglect that caused harm from unnecessary treatment for a cancer that was benign. These misdiagnosis situations might be considered "overdiagnosis" rather than "underdiagnosis," as discussed previously. Breast cancers have been estimated to be overdiagnosed as much as 31% of the time20--meaning that a woman's breast lump was not really cancer and was benign, or was only a precancerous tumor. The harm or injury in these types of overdiagnosis cases occurs when the patient is given surgery (such as mastectomy), chemotherapy, radiation and/or other unnecessary treatment(s).
Medical Malpractice Cases for Cancer Mistreatment
In addition to the above cancer misdiagnosis cases, there are also situations where the patient, though properly diagnosed with cancer, was given the wrong treatment, or inadequate treatment for the cancer. Depending on the situation, inadequate treatment can also cause injury or death due to the delay, and improper treatment (such as with excessive dose(s) of chemotherapy/drug therapy or radiation) can cause injury or death simply as a result of toxicity. These are also situations where negligent care that causes patient harm may be legally actionable.
The Lawyer's Role
The lawyer who is experienced in handling cancer misdiagnosis and mistreatment cases will know and understand the medicine and important medical literature on this subject. He or she will be able to work with qualified oncologists, radiologists, surgeons, pathologists and other expert witnesses to determine whether and why cancer misdiagnosis or mistreatment occurred, and if and why this caused significant injury or harm.
Contact Us
Attorneys at Clore Law Group have significant experience and expertise with handling cancer misdiagnosis and mistreatment cases to successful resolution. We have represented patients or their families in cases involving breast cancer, colon cancer, prostate cancer, skin cancer (melanoma), lung cancer, and lymphoma/leukemia, when the alleged cancer misdiagnosis or mistreatment was a cause of severe injury or death. Many times such cases involve significant delays in treatment (or in recognizing the harmful effects of mistreatment), leading to incurable cancer or premature death. We understand how these harmful errors are devastating not only for the patients who suffer them, but their families as well. If you think that you or a loved one may have experienced a tragic outcome from cancer misdiagnosis or mistreatment, you can email us at [email protected], or call us Toll-Free at 1-800-610-2546 for a free and confidential consultation.
Sources
- American Cancer Society (ACS), The History of Cancer, at: https://www.cancer.org/content/dam/CRC/PDF/Public/6055.00.pdf; and https://acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/cncr.22608.
- National Cancer Institute (NCI), at: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cancer.
- Id.
- See, e.g., https://www.cancerquest.org
- Note that carcinoma in situ (CIS) is not really yet a cancer, even though the cells look cancerous under a microscope, because it has not yet invaded into the organ from which it originated. See, e.g., NCI, at: https://www.cancer.gov/about-cancer/diagnosis-staging/staging.
- See, e.g., Adair TH, Montani JP. Angiogenesis, Ch. 1 Overview of Angiogenesis, San Rafael (CA): Morgan & Claypool Life Sciences (2010).
- See, e.g., NCI, at: https://www.cancer.gov/types/metastatic-cancer.
- Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/cancer/dcpc/prevention/screening.htm.
- See NCI, at: https://www.cancer.gov/about-cancer/diagnosis-staging/staging.
- See NCI, at: https://www.cancer.gov/about-cancer/diagnosis-staging/prognosis#factors.
- Burton, EC, Troxclair, DA., et al, Autopsy diagnosis of malignant neoplasms: how often are clinical diagnoses incorrect?, JAMA. 280(14):1245-8 (Oct. 14, 1998).
- See NCI for a cancer list, in descending order of frequency: breast, lung, bronchus, prostate, colon, rectum, melanoma, bladder, non-Hodgkin lymphoma…, at: https://www.cancer.gov/about-cancer/understanding/statistics.
- National Coalition on Healthcare and Best Doctors, Exploring Diagnostic Accuracy in Cancer: a Nationwide Survey of 400 Leading Cancer Specialists, Question 4, available at: http://www.qualitystar.net/wp-content/uploads/2014/09/QualityStar-Misdiagnosis-Survey.pdf.
- See Newman-Toker, DE., et al, in above bar chart, originally published online in July 2019, at: https://www.degruyter.com/document/doi/10.1515/dx-2019-0019/html.
- Unlike South Carolina, some states instead allow causation to be sufficient if there is a substantial lost chance of cure or survival due to the neglect. See, e.g., Hemminger v. LeMay, 2014 IL App (3d) 120392, modified upon denial of reh’g; Holton v. Mem’l Hosp., 176 Ill. 2d 95 (1997).
- Holland-Frei, Cancer Medicine, Ch. 1 by Folkman, J, Raghu, K., Beginnings of Angiogenesis Research, p. 6 (6th ed. 2003).
- See Talkington, A, Durrett, R. Estimating tumor growth rates in vivo, Bull Math Biol., 77(10): 1934–1954 (Oct. 2015). See also Detterbeck, FC, Gibson, CJ. Turning Gray, The Natural History of Lung Cancer Over Time, J. of Thorac. Oncol. 3(7): 781-792 (July 2008)(“simple mathematics correlates each doubling of volume with an increase in the diameter of approximately 1.26 (the cube root of 2)”). Id. at 787.
- For more information that explains the problems with defense lawyers use of estimated DTs, see https://www.meyersmedmal.com/understanding-the-tumor-doubling-defense/. Additionally, these defense arguments ignore the fact that many doublings are necessary before angiogenesis occurs, which is required for metastasis, and that some tumors can grow to one-few millimeters in size before they experience angiogenesis. Holland-Frei, Cancer Medicine, fn16 infra, Ch. 1, at 6-7.
- See infra, fns 16-18. Additional limitations of estimated DT may include the type of model (and formula) and its application to the facts, as well as the fact that DT models apply to primary, untreated, tumors; metastases, as mentioned, may double 2-3 times or more faster than a primary cancer tumor. Further, the lower limit of radiologic detectability of cancers may hinder attempts to acutally measure and calculate tumor size, since this depends on the type of cancer and imaging; some cancers may not be radiologically detectable until they are at least > 5 mm or more. See, e.g., Nukleer, TT, et al, Limits of Tumor Detectability in Nuclear Medicine and PET, Molec. Im. and Rad. Ther. 21(1):23-28 (2012); Hayashi, H, Ashizawa, K. Detectability of peripheral lung cancer on chest radiographs: effect of the size, location, and extent of ground-glass opacity, Br. J. Radoiol. 82;976 (Jan. 28, 2014). Likewise, very short interval times between imaging studies may be insufficient from which to accurately derive (calculate) DTs. See, e.g., Mehrara, D, Forssell-Aronsson, EF, Specific Growth Rate versus Doubling Time for Quantitative Characterization of Tumor Growth Rate, Cancer Res., 67(8): 3970-75 (Apr. 15, 2007).
- Bleyer, A, Welch, HG. Effect of Three Decades of Screening Mammography on Breast-Cancer Incidence, N. Engl. J. Med. 367: 1998-2005 (Nov. 12, 2012).