Brain Injury or Paralysis From Malpractice in Seated Surgeries

Believe it or not, in certain surgeries the way your body is positioned can be more dangerous than the operation itself. The reason is that in some surgeries, particularly of the spine, upper torso, shoulder, or head, the surgeon may want you in a seated or upright-type of position, so that he or she has better access to the operative area. In seated positions, the level of your head will of course be above the level of your heart; so, the effects of gravity mean that while your blood pressure may be okay during surgery at the level of your heart, it can be dangerously low at the level of your neck (spinal cord) and head (brain). Danger can occur due to low blood pressure from the combined effects of: (1) general anesthesia, which dilates blood vessels and dampens the heart's ability to compensate by pumping faster and harder, (2) drugs that are often given during surgery to keep your blood pressure low to begin with, because this lessens bleeding and makes it easier for the surgeon to operate, and (3) your heart having to pump the blood not only throughout your body but also uphill as well--so that it can carry oxygen through the circulation into the spinal cord and brain.1 Moreover, if the surgeon is operating and manipulating tissues and blood vessels in an area that supply blood to the central nervous system (i.e. CNS -- spinal cord and brain), this compounds the effects because the blood flow (which is already lower in that area) can be slowed even further by compression of these vessels.2 If the dangerously low blood pressure and flow is not timely and properly-recognized and corrected for the patient in a seated position, it may have catastrophic consequences of causing paralysis, brain damage or stroke from lack of oxygen (i.e. hypoxia) and/or low oxygen blood flow (i.e. ischemia) to the spinal cord or brain.3 This can amount to medical malpractice, in particular by the anesthesia provider.
The Surgical Position
There are many positions that a patient may be placed in, depending on the nature and type of surgery. Below are simple illustrations of common ones:
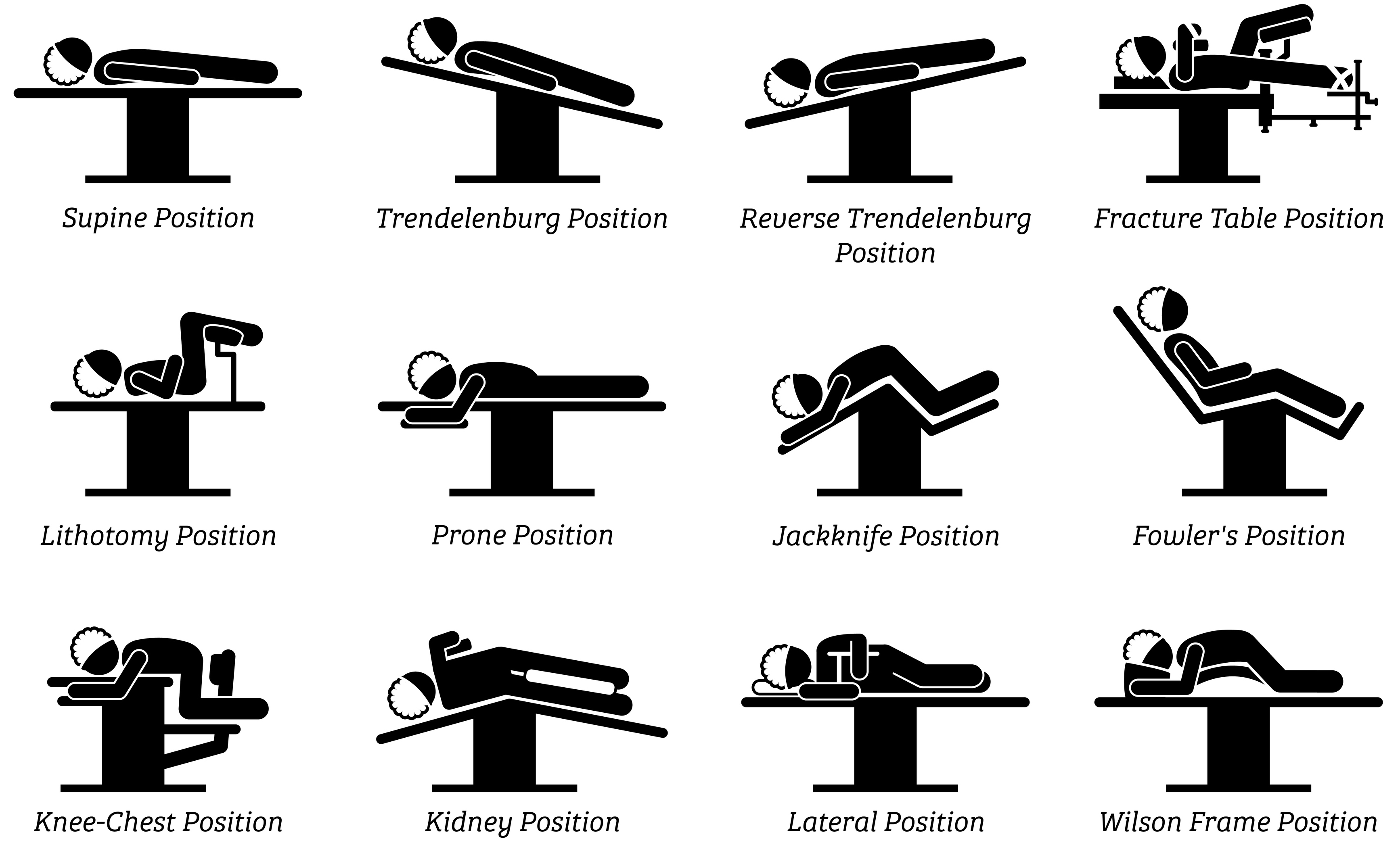
The two surgical positions above that are worrisome for dangerously low blood pressure to the brain can quickly be identified since they are the ones where the neck and head are elevated higher than the heart: (1) Fowler's (also known as "beach chair" or "barbershop" position)4 and (2) Trendelenburg positions, or variations of those positions.5
 Blood Pressure Changes in Upright Positions
Blood Pressure Changes in Upright Positions
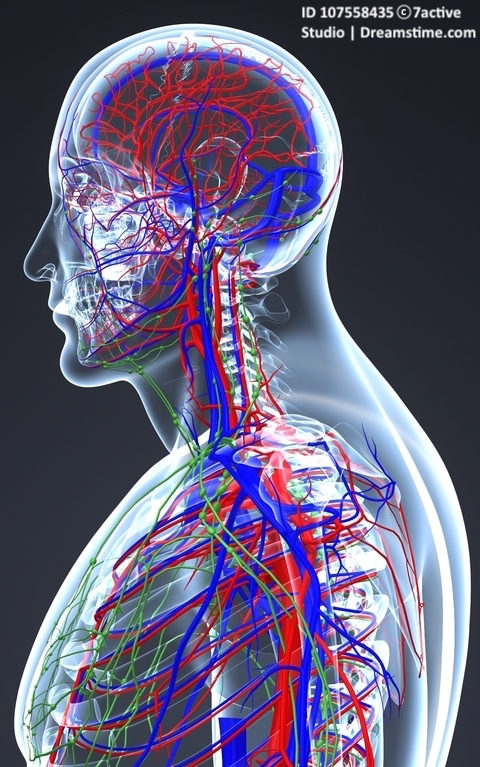
The circulatory system has a vast, rich network of blood vessels, including above the heart that carry blood to the spinal cord and brain (arteries--in red), and that carry blood back from the spinal cord and brain to the lungs (veins--in blue) where it is re-oxygenated and sent back to the heart to be pumped out again. When we are seated, standing or upright in daily life, our heart is constantly pumping blood through our circulatory system, including into arteries that supply our spinal cord and brain. Basic human physiology allows and compensates for this, or else we would have dangerously low blood pressures above the heart all the time when we are upright. Sometimes, however, blood pressure can suddenly get too low, especially in the sick or elderly, if they quickly sit or stand up. This is known as orthostatic or postural hypotension--meaning that blood pressure usually drops quickly about 20 points in the upper number (systolic) or 10 points in the lower number (diastolic), which are measured in millimeters of mercury (mm Hg). And if someone has postural hypotension, they can suddenly get a headache, become dizzy or faint from the effects of the low blood pressure. This happens upon the sudden change in posture because gravity causes blood to pool in the lower part of the body, and thereby lowers the amount and flow of blood going into the upper part of the body. The rapid change means that suddenly there is less blood flow and oxygen going to the brain.6
Blood Pressure vs. Blood Flow
Blood pressure, however, is not necessarily the same as blood flow. Blood pressure means the pressure exerted on the arteries by the blood pumped from the heart. Blood flow depends not just on the amount of pressure, but also the resistance of the blood vessels. Think of it this way: when you turn the knob on your garden hose, it increases the water pressure in the hose. This also increases the water flow, assuming that the hose is open. But what if the hose is kinked? If you dial up the knob, the water pressure will be increased but not the flow out of the hose. But if you rapidly open it, the flow comes rushing out and is greatly increased. By the same token, what if the hose is open but is so large in diameter (like a fireman's hose) that the knob from your home water supply has to be turned wide open just to get the hose to partially open, so that only a small amount of water flows out? Or what if you hold the hose straight up? The water flow will also be much less the further it has to travel upward. Mathematically, blood flow equals blood pressure divided by blood resistance.7 Gravity is a form of resistance, of course, and therefore requires greater blood pressure to increase blood flow. For surgery, doctors measure blood pressure in terms of mean arterial pressure (MAP) to have a single number, which is a calculation made from both the upper (systolic) and lower (diastolic) blood pressures.8 For instance, a blood pressure of 120/80 equals a MAP of 93.
the knob on your garden hose, it increases the water pressure in the hose. This also increases the water flow, assuming that the hose is open. But what if the hose is kinked? If you dial up the knob, the water pressure will be increased but not the flow out of the hose. But if you rapidly open it, the flow comes rushing out and is greatly increased. By the same token, what if the hose is open but is so large in diameter (like a fireman's hose) that the knob from your home water supply has to be turned wide open just to get the hose to partially open, so that only a small amount of water flows out? Or what if you hold the hose straight up? The water flow will also be much less the further it has to travel upward. Mathematically, blood flow equals blood pressure divided by blood resistance.7 Gravity is a form of resistance, of course, and therefore requires greater blood pressure to increase blood flow. For surgery, doctors measure blood pressure in terms of mean arterial pressure (MAP) to have a single number, which is a calculation made from both the upper (systolic) and lower (diastolic) blood pressures.8 For instance, a blood pressure of 120/80 equals a MAP of 93.
Blood Pressure in the Seated Surgical Position
When MAP is measured or calculated in surgery, it reflects the pressure at the level of the blood pressure cuff, not above it. So, when the patient is in a seated position, with the blood pressure cuff on the arm and therefore at around the same level as the heart, we know because of gravity that the MAP and the blood flow will be less at the level of the neck and head. The question is how to account for this difference that doctors call the hydrostatic pressure gradient. The conversion formula to determine this hydrostatic gradient, i.e. what the MAP is at a given level above the blood pressure cuff, is .77 mm Hg less for every 1 cm of upward change in elevation.9 In non-metric terms, this means for every 1" increased in elevation above the blood pressure cuff, the mean arterial blood pressure will drop 1.95 mm Hg.
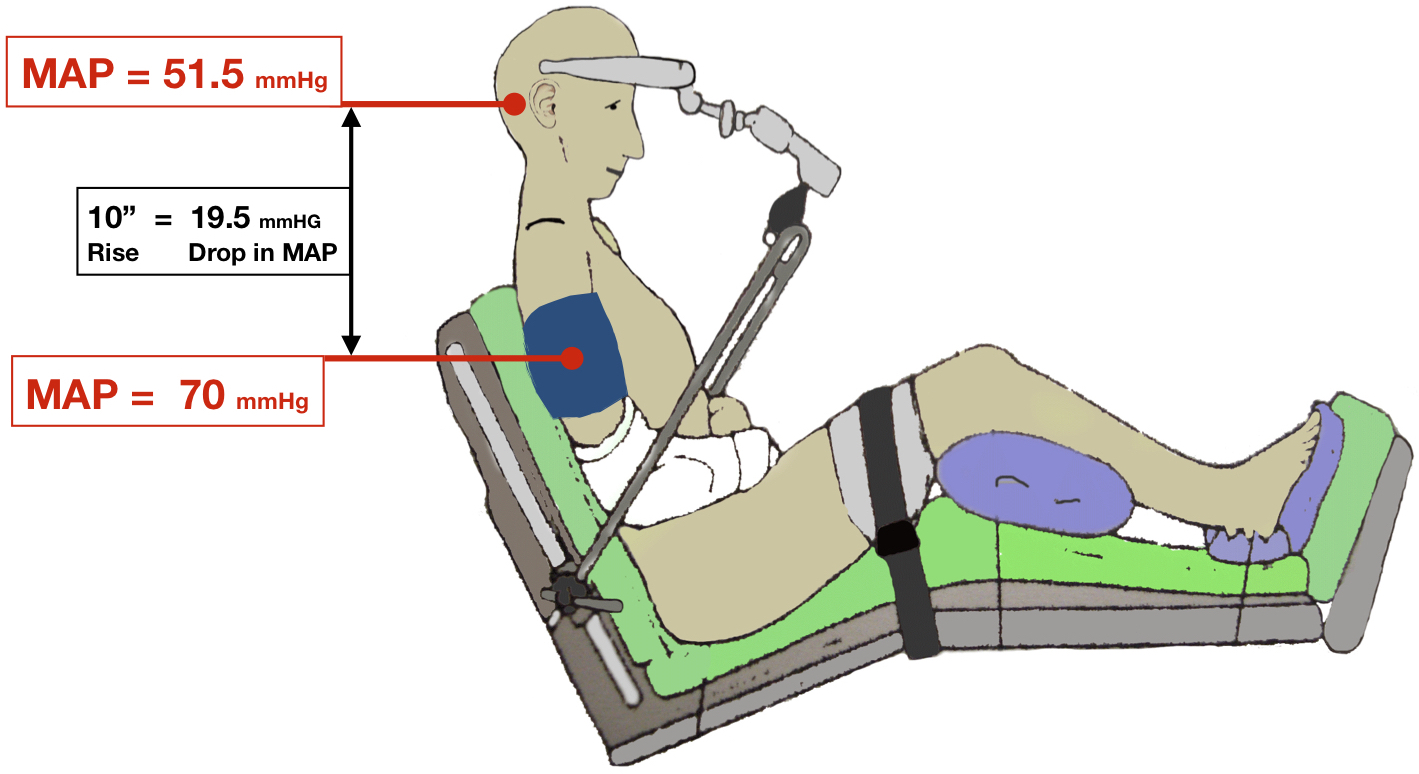
Illustration at Wikimedia (CC BY 1.0)
Brain and Spinal Cord Blood Flow in the Seated Position
The process by which adequate and stable blood flow is maintained for the brain despite wide changes in blood pressure is called "cerebral autoregulation."10 While most of our body systems and blood vessels regulate blood flow to organs, the brain is very sensitive to too much or too little blood flow, in part because it has higher demands for oxygenated blood and nutrients. So, the process by which blood flow is automatically regulated for the brain depends on how much blood, oxygen, and nutrients are carried to and from the brain as well as what things change the flow-regulating mechanisms. It is well-known in medicine that when patients are moved to an upright position, the MAP, heart rate, and amount of blood in and pumped from the heart, decreases, in addition to other changes .11 In patients not under general anesthesia, the body and blood vessels compensate for this to increase the pressure and flow, but under general anesthesia the autoregulation capability is reduced and we cannot do so to the same degree; and, blood pressure decreases in the patient who is in a seated position. Likewise, the amount of blood flow actually perfusing the brain, known as "cerebral perfusion pressure" (CPP) decreases by about 15% in upright patients even before they are given anesthesia.12 It is also well-understood in medicine that there is a lower limit or threshold necessary to maintain cerebral autoregulation‚ meaning that if the CPP falls below a certain level, the constant blood flow needed by the brain cannot be regulated, and brain injury, or paralysis from damage to the spinal cord, can occur from hypoxia/ischemia. CPP is the MAP minus the amount of resistance in the skull from the brain and fluid, which is called intracranial pressure (ICP). ICP is normally 5 – 15 mm Hg. The extreme lower limit of CPP for cerebral autoregulation is 50 mm Hg, but some people may require CPP to be as high perhaps as 70-80 mm Hg or so to maintain autoregulation, particularly if they have prior high blood pressure (hypertension).13 What all this means is that during surgery in the seated position, it is generally believed that patients can have brain injury, stroke or paralysis from a CPP of < 50 - 70 mm Hg, and so anesthesia providers have to monitor these patients' blood pressures continually during surgery, and make sure they are given drugs to raise the blood pressure if necessary. If in doubt, the anesthesia provider should err on the side of caution,14 but an excessively high blood pressure can also be a problem.
and blood vessels regulate blood flow to organs, the brain is very sensitive to too much or too little blood flow, in part because it has higher demands for oxygenated blood and nutrients. So, the process by which blood flow is automatically regulated for the brain depends on how much blood, oxygen, and nutrients are carried to and from the brain as well as what things change the flow-regulating mechanisms. It is well-known in medicine that when patients are moved to an upright position, the MAP, heart rate, and amount of blood in and pumped from the heart, decreases, in addition to other changes .11 In patients not under general anesthesia, the body and blood vessels compensate for this to increase the pressure and flow, but under general anesthesia the autoregulation capability is reduced and we cannot do so to the same degree; and, blood pressure decreases in the patient who is in a seated position. Likewise, the amount of blood flow actually perfusing the brain, known as "cerebral perfusion pressure" (CPP) decreases by about 15% in upright patients even before they are given anesthesia.12 It is also well-understood in medicine that there is a lower limit or threshold necessary to maintain cerebral autoregulation‚ meaning that if the CPP falls below a certain level, the constant blood flow needed by the brain cannot be regulated, and brain injury, or paralysis from damage to the spinal cord, can occur from hypoxia/ischemia. CPP is the MAP minus the amount of resistance in the skull from the brain and fluid, which is called intracranial pressure (ICP). ICP is normally 5 – 15 mm Hg. The extreme lower limit of CPP for cerebral autoregulation is 50 mm Hg, but some people may require CPP to be as high perhaps as 70-80 mm Hg or so to maintain autoregulation, particularly if they have prior high blood pressure (hypertension).13 What all this means is that during surgery in the seated position, it is generally believed that patients can have brain injury, stroke or paralysis from a CPP of < 50 - 70 mm Hg, and so anesthesia providers have to monitor these patients' blood pressures continually during surgery, and make sure they are given drugs to raise the blood pressure if necessary. If in doubt, the anesthesia provider should err on the side of caution,14 but an excessively high blood pressure can also be a problem.
How Anesthesia Providers Can Calculate the Blood Pressure/Flow Variation at the Brain & Spinal Cord
Blood pressure cuffs used during surgery will display the systolic and diastolic blood pressure numbers, as well as the MAP (usually in parenthesis), on a monitor. If the cuff is applied to the arm or leg, the difference between the MAP at that level versus the level of the spinal cord and brain must be calculated by the anesthesia provider. To do this, the conversion factor discussed above or a similar formula must be used. This tells the anesthesia provider, who is responsible for monitoring, what the blood pressure is (compared to what it should be) at the central nervous system level, and whether or not the patient needs to be given drugs to raise the blood pressure. Sometimes this requires ongoing discussion with the surgeon, who may be concerned about higher blood pressures causing excessive bleeding. But the anesthesia provider has to realize that if the patient has a MAP, for example, of 65 mm Hg at the level of the arm cuff and the patient's head is 10" above that level, then the MAP is only 45.5 mm Hg at the level of the brain, which for some patients may be way too low, making the CPP even less (i.e. 45.5 – 5 to 15 = CPP of 30.5 to 40.5 mm Hg), which can cause brain damage, stroke or paralysis to the patient from hypoxia/ischemia.
How Anesthesia Providers Can Monitor the Blood Pressure/Flow Variation at the Brain & Spinal Cord
An easier way to know the MAP during the surgery, without having to use a conversion factor or formula, is simply for the anesthesia provider to insert a small tube (catheter) into the radial  artery in the wrist (or another peripheral artery) to measure it (see photo). This device has a transducer attached, which can be placed at the desired height, such as the level of the patient's head. This results in the MAP being measured and displayed on the monitor at the level the transducer, rather than at the level of a blood pressure cuff on the arm or leg.
artery in the wrist (or another peripheral artery) to measure it (see photo). This device has a transducer attached, which can be placed at the desired height, such as the level of the patient's head. This results in the MAP being measured and displayed on the monitor at the level the transducer, rather than at the level of a blood pressure cuff on the arm or leg.
With this device, the anesthesiologist simply needs to remember that the CPP will be 5-15 mm Hg less than the MAP recording that is displayed on the monitor. In many shoulder or torso surgeries, however, this equipment may not be available to measure the MAP directly, in which case the conversion formula for the hydrostatic gradient must be used.15
Brain and Spinal Cord Injury
As noted previously, it has been known for many years that patients in seated surgical positions can experience paralysis or brain damage/stroke from low blood pressure, and thus low CPP, resulting in lost cerebral autoregulation. Deliberately keeping blood pressures low simply to appease the surgeon can be dangerous when the beach chair or similar position is used. Experts in anesthesiology point out that typically the surgeon and the anesthesiologist or CRNA don't consider the added effect of the beach chair position on cerebral perfusion.16 These same experts advise:
"If we have to undergo shoulder surgery in the beach chair position, we'll make every effort to ensure that our anesthesiologist maintains a safe and appropriate CPP well above 50 mm Hg. In so doing, we would rather be safe than sorry. Other patients deserve no less."17
The Lawyer's Role
The lawyer who is experienced in prosecuting medical malpractice cases involving operations that result in brain injury, stroke or paralysis will know and understand the importance of the patient's blood pressure and positioning (or posture) during the surgery. The lawyer should understand these concepts, the anatomy, the need for the maintaining MAP and CPP, and important literature on these subjects. He or she will be able to work with qualified anesthesiologists, CRNAs, surgeons and other expert witnesses to determine if and whether low blood pressure or flow caused or contributed to a central nervous system injury, in addition to whether or not the surgery itself was a causative factor. By working with these experts, the lawyer will be able to analyze whether the tragic outcome of brain injury, stroke or paralysis could and should have been avoided with a proper and timely care during surgery.
Contact Us
The attorneys at Clore Law Group have extensive experience and expertise with surgical cases resulting in brain injury and paralysis. This includes the situation where low blood pressure and flow in a seated surgical position resulted in central nervous system injury. If you or a loved one suffered and injury like this during surgery, and you have any reason to question the care, including the blood pressure or positioning in surgery, you can email us at [email protected], or call us Toll-Free at 1-800-610-2546 for a free and confidential consultation.
Sources
- See, e.g., Cullen DJ, Kirby RR, Beach Chair Position May Decrease Cerebral Perfusion, Newsletter: The Official Journal of the Anesthesia Patient Safety Foundation, Vol. 22, No. 2, pp. 25-40 (Summer 2007), which can be accessed at: https://www.apsf.org/newsletter/summer-2007/.
- Id. at 27 (noting articles suggesting that blow flow to the brain can be compromised by mechanical obstruction or injury to the major arteries or veins as well). See also Hindman BJ, Palecek JP, et al, Cervical spinal cord, root, and bony injuries: a closed claims analysis, Anesthesiol. Vol. 114, No. 4, pp. 782-95 (Apr. 2011).
- Id. See also Pohl A, Cullen DJ, Cerebral ischemia during shoulder surgery in the upright position: a case series, J Clin Anesth. Vol. 17, No. 6, pp. 463-69 (Sep. 2005); Neligan P, Beachchair and Blood Pressure, AnesthesiaWest (Jan. 24, 2013), at: https://anaesthesiawest.wordpress.com/2013/01/24/beachchair-and-blood-pressure/.
- Id.
- Id. Also note that the sitting position in surgery increases the risk of serious neurological and other injuries due to air embolism. Porter JM, Pidgeon C, et al, The sitting position in neurosurgery: a critical appraisal, Br J Anaesth. Vol. 82, No. 1, pp. 117-28 (Jan. 1999).
- See, e.g., Wedro B, Orthostatic Hypotension (Low Blood Pressure When Standing), at: https://www.medicinenet.com/orthostatic_hypotension/article.htm#orthostatic_hypotension_definition_and_facts; Messerli FH, Cardiovascular Disease in the Elderly, Ch. 8, Postural Hypotension and Syncope in the Elderly, by Ziegler MD, Barager RR, pp. 129-46 (Springer Boston, MA 2d ed. 1988).
- See, e.g., Pollock JD, Makaryus AN, Physiology, Cardiovascular Hemodynamics, NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health (NIH), (Jan. 2018), at: https://www.ncbi.nlm.nih.gov/books/NBK470310/.
- A formula to calculate the MAP from regular systolic and diastolic blood pressures is: MAP = [(2 x diastolic) + systolic]/3. See, e.g., https://globalrph.com/medcalcs/mean-arterial-pressure-map/.
- Cullen DJ, Kirby RR, Beach Chair Position May Decrease Cerebral Perfusion, n1, at 27.
- See, e.g., Cipolla MJ, The Cerebral Circulation (2009), at Ch. 5, Control of Cerebral Blood Flow, sec. Autoregulation of Cerebral Blood Flow; OpenAnesthesia, at: https://www.openanesthesia.org/aba_cerebral_autoregulation/.
- Cullen DJ, Kirby RR, Beach Chair Position May Decrease Cerebral Perfusion, n1, at 25.
- Id.
- Id.; Newfield P, Cottrell JE, Handbook of Neuroanesthesia, p. 365 (LWW 4th ed. 2007); Drummond JC, The Lower Limit of Autoregulation: Time to Revise Our Thinking?, Anesthesiol. Vol. 86, No. 6, pp. 1431-33 (Jun. 1997); Cerebral Autoregulation website, at: http://www.cerebralautoregulation.com/node/8; and, Cullen DJ, Kirby RR, Lower Limit of Cerebral Autoregulation Questioned, Newsletter: The Official Journal of the Anesthesia Patient Safety Foundation, Vol. 24, No. 1, p. 5 (Spring 2009), at: https://www.apsf.org/newsletter/spring-2009/.
- Lanier WL, Cerebral Perfusion: Err on the Side of Caution, Newsletter: The Official Journal of the Anesthesia Patient Safety Foundation, Vol. 24, No. 1, pp. 1-4 (Spring 2009), at: https://www.apsf.org/newsletter/spring-2009/.
- Cullen DJ, Kirby RR, Beach Chair Position May Decrease Cerebral Perfusion, n1, at 27. 16 Id. at 25 & 27. 17 Cullen DJ, Kirby RR, Lower Limit of Cerebral Autoregulation Questioned, n13, at 5.