Airway Medical Malpractice—Part I of III: Failure to Anticipate the Difficult Airway

When a healthcare practitioner places a breathing tube in a patient's airway,1 most of us think of it as routine--what could go wrong? In truth, this can turn out to be a dangerous situation more often than you might think. One problem is that in some patients it is difficult to get the breathing tube (i.e. an endotracheal or ET tube) down the throat and into the patient's windpipe (trachea).2 The reasons for difficulty in this process, known as endotracheal intubation, include the patient's anatomy, e.g. variant size or shape of structures like the tongue, palate, voice-box, throat, neck, or jaw, etc., as well as other medical abnormalities or conditions that can impact the airway, such as birth defects, trauma, cancer, sleep apnea, pregnancy, obesity, prior surgery, or an already blocked airway (emergencies) or other reason for a difficult airway.3 The practitioner who has time to evaluate the patient for these issues before intubation, but who does not properly do so, may lose a significant opportunity to anticipate and avoid a difficult or harmful intubation.4 Harm can occur from medical malpractice when the unconscious or anesthetized patient is not timely intubated at a time when the practitioner also cannot get air movement in and out of the lungs with an air mask (i.e. ventilation), which can cause brain injury within minutes from a lack of oxygen (anoxia), followed by death.5
Why is Intubation Performed?
Common reasons for intubation are:
- To keep the airway open and provide oxygen in surgery with general anesthesia
- To keep the airway open and provide oxygen in deep sedation procedures
- To recover from serious injury or illness if longer sedation is needed
- To protect the lungs and/or the airway
- To protect the airways of patients who may not be able to do so
- To ensure no obstruction of the airway will prevent oxygenation and breathing
- If the patient has stopped breathing or has difficulty breathing
- If the patient needs a machine (ventilator) to help breathe
- If the patient has a head injury and cannot breathe on his or her own
What are the Dangers?

If intubation difficulties persist, or failure recurs, despite repeated attempts, when the anesthetized or unconscious patient cannot breathe or effectively be given oxygen by facemask in the meantime, the situation is known as "cannot intubate, cannot ventilate," and it carries the highest anesthesia risk of brain damage and death.6
What is a Difficult Airway?
There is no real standard definition for the terms "difficult airway." There are three principal medical specialties in the U.S. that have and use different meanings for the terms: (1) anesthesiology, (2) emergency medicine, and (3) intensive care medicine. The reason for the differences in meaning of the terms relates in part perhaps to the different situations in which these two groups of healthcare providers often encounter airway difficulty--with anesthesia providers this occurs many times before surgery begins, whereas with emergency healthcare providers the situation may arise upon encountering the unconscious, trauma or allergic/anaphylactic patient. The intensive healthcare provider usually takes care of patients in the intensive care unit, but may be called to a regular ward (floor) to assist with airway management. The American Society of Anesthesiologists (ASA) refers to "difficult airway" for anesthesia providers as follows: "the clinical situation in which a conventionally trained anesthesiologist experiences difficulty with facemask ventilation of the upper airway, difficulty with tracheal intubation, or both."7 In the field of emergency medicine, leading authorities refer to "difficult airway" as meaning "one in which identifiable anatomical attributes predict technical difficulty with securing the airway.8
Failure to Anticipate the Difficult Airway
Oftentimes, a practitioner can anticipate beforehand that there will be difficulty in placing the breathing tube or in making sure there is air movement in and out of the chest. The ability to recognize potential airway difficulty basically depends on two factors: (1) the opportunity the practitioner has to obtain information, examine the patient and inspect the airway; and, (2) how careful the practitioner is in doing these things. A failure to do either of these things properly can amount to medical malpractice.
The Patient Who Had Airway Difficulty in the Past
If someone has a physical reason or condition that made it difficult in the past for a health care provider to intubate or ventilate them, then there is a good chance there will be difficulty again when another practitioner tries to do so--assuming the physical reason or condition still exists. So, past airway difficulty strongly predicts future airway problems.9 This is why anesthesia providers should ask the patient about this type of information (i.e. history) before surgery. Emergency care givers, however, may not have the ability to do this, particularly when confronted with an unconscious patient or one who cannot communicate.
The Patient Whose Medical Condition Suggests Airway Difficulty
As previously noted, a number of abnormalities of the airway due to medical conditions or disorders can suggest, and sometimes strongly indicate, there will be airway difficulty. One of the most common questions the anesthesia provider should ask about during the history is if the patient has sleep apnea or snoring problems. When we sleep, our throat structures relax. With sleep apnea, a person has episodes during sleep of snoring and their tongue usually falls back against the soft palate, and the soft palate and uvula fall back against the back of the throat, resulting in the airway being blocked.10
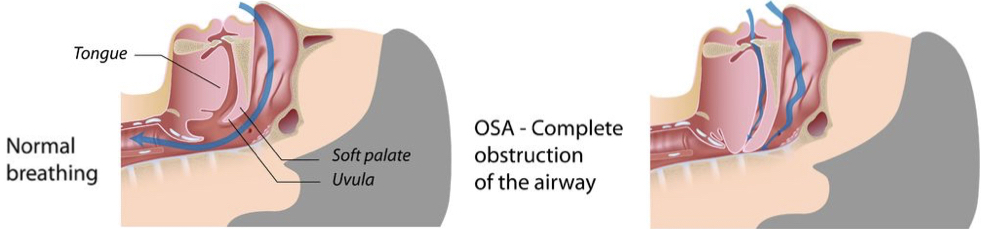
So, this is medically termed "obstructive" sleep apnea (OSA). Unlike anesthesia providers, emergency care providers may not be able to learn of this information from the patient, or from a family member if no one is with the patient at the time. So, the amount of information the practitioner can get as to a person's prior medical conditions that could impact the airway depends on the circumstances. In fact, when emergency medicine physicians are confronted with an unconscious patient on the verge of death, they follow a "crash" airway plan, by maintaining oxygenation and going straight to the scope in order to intubate.11
The Patient Whose Anatomy Poses Airway Difficulty
An important purpose of an anesthesia provider's initial pre-operative evaluation of the patient is to examine the patient to try detect the likelihood of a difficult airway. While the emergency practitioner may have less time to inspect the patient in life-and-death situations, there are several physical signs that, if present, strongly suggest to all practitioners a difficult intubation,12 including:
- Short, muscular neck
- Receding lower jaw
- Protruding front teeth
- Poor ability to open the jawbone
- Long, high-arched roof of the mouth
- Decreased neck movement
- Short distance from the chin to the notch at the Adam's apple
The anesthesia practitioner planning to perform intubation can look into the patient's mouth before surgery to determine the Mallampati classification (named for the doctor who created it), which is a rough estimate of the tongue size relative to the oral cavity. Although the single usage of this bedside screening classification has limited ability to help anticipate a difficult tracheal intubation,13 it is a simple, reproducible and reliable preanesthetic airway assessment when properly performed. On the other hand, the emergency medical practitioner may be presented with a patient who cannot sit up or follow instructions to allow the best view inside the patient's mouth, and thus may only get a rough Mallampati assessment.14
The Mallampati classification that practitioners use today is a modified one that has four different classifications to gauge the visibility of the amount of soft palate and soft hanging flap (uvula) at the back middle of the throat, and thus the potential ease of intubation.15 As seen with the illustration below, the larger the tongue size, the more difficult it is see these structures. So, a Mallampati class I score gives the most room to see these landmarks and intubate, while a class IV gives the least.
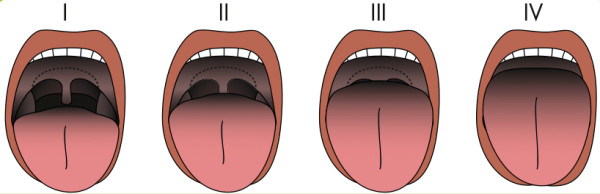
Credit: Illustration from Incidence of unanticipated difficult airway using an objective airway score versus a standard clinical airway assessment, by © Norskov AK, et al, Trials 2013 14:347, Fig. 3; licensee BioMed Central Ltd. 2013, (CC BY 2.0).
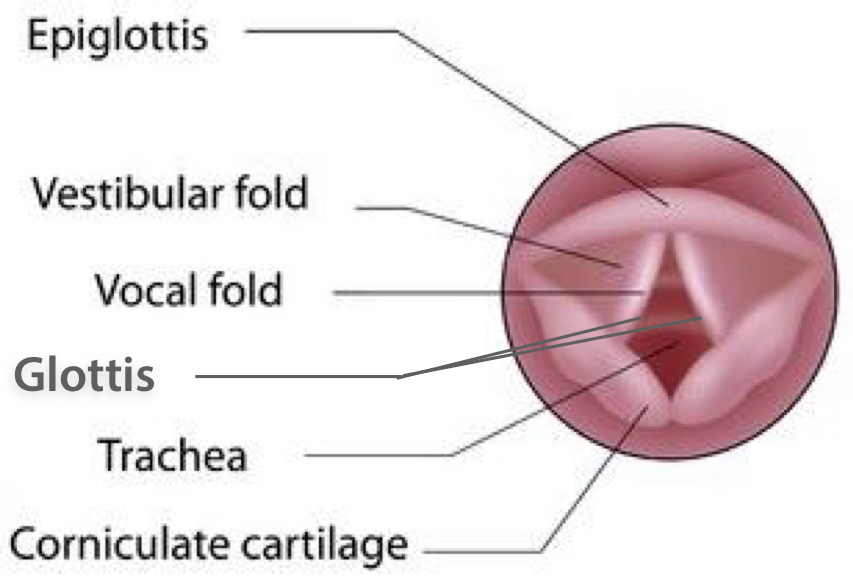
The modified Mallampati test can have good accuracy in predicting difficult intubation, and a score of III-IV has been associated with both sleep apnea and difficult mask ventilation.16 When certain anatomical characteristics are combined with the modified Mallampati assessment, the ability to predict a difficult intubation increases.17 In addition to a Mallampati assessment, a further way for all practitioners to evaluate for a difficult airway is to look deeper inside the throat, with the use of a device known as a laryngoscope. This is an important opportunity for all practitioners who are planning to intubate, before they actually do so, i.e. prior to actually placing the ET tube. Laryngoscopes have a light, with a metal blade (curved or straight) attached. After a muscle relaxant or anesthetic is given (depending on the circumstances) the laryngoscope blade is inserted to keep the tongue depressed and out of the line of sight, and then it is used to lift up the throat flap in front of the wind-pipe (epiglottis) that keeps food from going down it, to see down into the voice-box (larynx) area. Specifically, the blade goes all the way into the depression just behind the root of the tongue (vallecula) to directly visualize the opening between the vocal cords (glottis). Once this is identified, then the ET tube can be inserted through the vocal cords (folds).
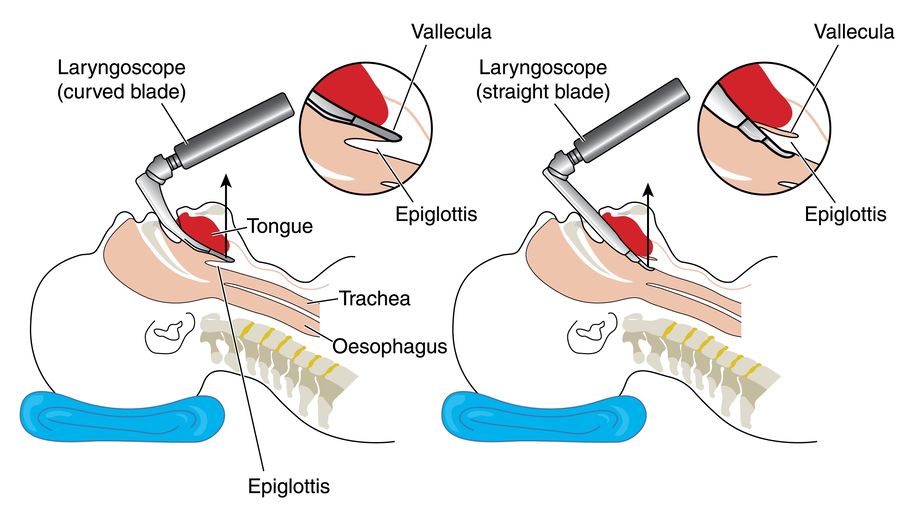
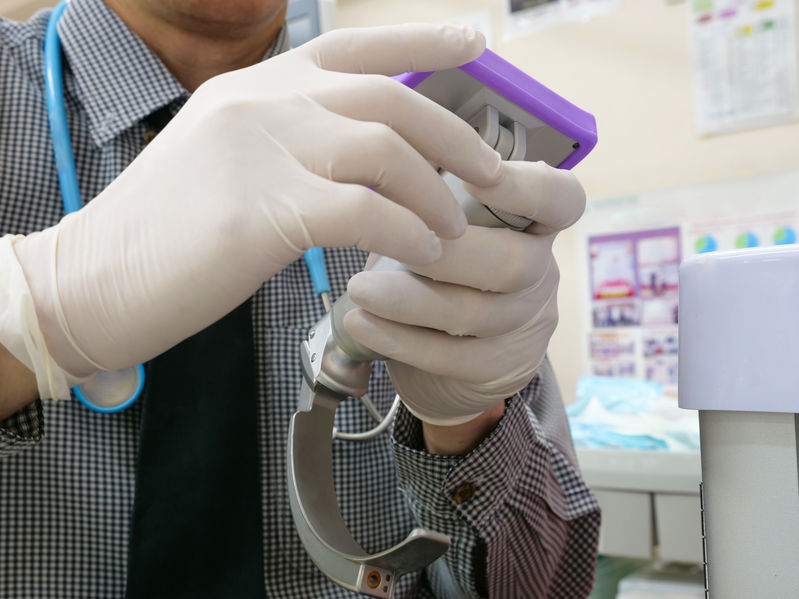
Many laryngoscopes today have video-assisted technology, where a small camera is mounted to the top of the metal handle, to allow for even better visualization of these structures, as seen to the right. The ability to classify the airway, and predict the difficult airway, is more accurate based on this system.18
Direct laryngoscopy in and of itself, before any attempt to insert the breathing tube, is difficult in 1/25 to 1/100 patients with a class III Cormack-Lehane (CL) score, and impossible in 1/285 to 1/2000 patients who have a class III-IV CL score, which commonly makes traditional intubation impossible as well.19 In sum, the assessment during laryngoscopy, before the attempted insertion of a breathing tube, gives a good idea of whether or not the breathing tube can or cannot be inserted; it also lets the practitioner recognize that different airway options or equipment may need to be used. Likewise, facemask ventilation is estimated to be difficult with anesthetics in about 1/50 to 100 cases, and impossible in about 1/500 cases. But a CL score of III-IV with laryngoscopy, as well as snoring (sleep apnea), increases the risk of ventilation problems.20 The problem with repeated attempts to perform laryngoscopy or intubation is that forceful airway manipulation, including with the metal blade(s), can convert a situation where ventilation was possible (even though intubation was not), into the emergency situation where neither the intubation nor the ventilation is possible.21
This can constitute medical malpractice. So, practitioners should take all this type of information into account, time permitting, before deciding on the best strategy and plan for how to achieve intubation and ventilation, especially in the patient at risk for a difficult airway. Emergency medicine practitioners who face limited examination and/or laryngoscopy time are advised by experts in the field to use a simple word (LEMON) to help them remember the important physical (anatomical) signs the patient has, which should be used as a guide to quickly and reliably identify as much as they can as to the risks of a difficult airway.22 The pneumonic is:
Look externally: e.g. jaw, tongue, teeth, neck, face, etc.
Evaluate: i.e. observe the geometrical shapes of these structures in relation to one another, in particular the mouth opening, jaw space, and the position of the glottis in relation to the base of the tongue.
Mallampati Score: see above
Obstruction/Obesity: 4 signs of an upper airway obstruction are: muffled voice, difficulty swallowing, high-pitched wheezing, or feeling short of breath. Also, obesity may make it harder to see the glottis with the laryngoscope.
Neck Mobility: i.e. head or neck trauma, immobilization or restriction may prevent the best inside view, in which case video laryngoscopy is suggested.
Avoiding Medical Malpractice
By understanding and evaluating the risks for a difficult airway, practitioners who intubate or ventilate can have a better strategy and better options, and can use more advanced airway equipment if necessary, so as to make sure the patient is oxygenated and ventilated. The failure to do so may amount to negligence or medical malpractice, and can lead the practitioner down a dangerous path for the patient--a path that can ultimately result in a cannot-intubate-or-ventilate situation. This should always be avoided if possible and, as we'll discuss in part II of this three part series on airway medical malpractice, there are different options for how practitioners can avoid this danger and the disaster before intubation, as well as how to react after unsuccessful intubation when the patient can still be ventilated.
The Lawyer's Role
The lawyer who is experienced in prosecuting medical malpractice cases involving airway disasters, including intubation and ventilation deviations, will be able to evaluate and analyze the records and evidence concerning these matters, and medical literature about these subjects. He or she will be able to work with qualified anesthesiologists, emergency medicine physicians, and other expert witnesses to determine, and prove, if there was a failure to anticipate a difficult airway, why, and whether that was an important factor in the case of a tragic outcome like brain injury or death.
Contact Us
The attorneys at Clore Law Group have extensive experience and expertise with handling airway-related medical malpractice cases to successful resolution. This includes cases against various practitioners responsible for intubation, mask ventilation, and the emergency or surgical airway. If you think that you or a loved one may have experienced a tragic outcome like this from improper care , you can email us at [email protected], or call us Toll-Free at 1-800-610-2546
Sources
- Various physicians routinely intubate patients, including anesthesiologists, emergency medicine doctors and others, and the practice also commonly includes certified registered nurse anesthetists (CRNAs), anesthesiologist assistants, respiratory therapists, and certain other nurses and paramedics, as well as others who may be credentialed and/or licensed to do so.
- The estimated incidence is around 1/18 to 1/100 people who are difficult to intubate, and unsuccessful or failed intubation rates range from 1/100 in emergency room patients, 1/250 – 1/750 in obstetric patients, and anywhere from 3/1000 to 1/2230 of surgical patients, depending on which studies you look at. See Hagberg CA, Hagberg and Benumoff's Airway Management, Ch. 8, Definition and Incidence of the Difficult Airway, by Klock PA, pp. 178-82, and Ch. 9, Airway Assessment and Prediction of the Difficult Airway, by Anderson J, Klock PA, p. 193 (4th ed. Mosby 2018). See also Samsoon GL, Young JR, Difficult tracheal intubation: A retrospective study, Anaesth. Vol. 42, p. 487 (1987); Rocke DA, Murray WB, et al, Relative risk analysis of factors associated with difficult intubation in obstetric anesthesia. Anesthesiol. Vol. 77, p. 67 (1992); Hagberg CA, Handbook of Difficult Airway Management, p. 16 (Churchill Livingston 2000).
- Hagberg CA, Hagberg and Benumoff's Airway Management, n2, Ch. 9, by Anderson J, Klock PA, at 185-93; Practice Guidelines for the Management of the Difficult Airway: An Updated Report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway, Anesthesiol. Vol. 118, No. 2, pp. 251-70, at 254 (Feb. 2013).
- See, e.g., Bucher J, Cuthbert D, et al, The Difficult Airway: Common Errors During Intubation, eM Docs Practice Updates (June 19, 2016), at: http://www.emdocs.net/difficult-airway-common-errors-intubation/; Higgs A, McGrath, BA, et al, Guidelines for the management of tracheal intubation in critically ill adults, Br J Anesthes., Vol 120, No. 5, pp. 1137-38 (May 2018).
- See, e.g., Hagberg CA, Hagberg and Benumoff's Airway Management, n2, Ch. 8 by Klock PA, at 178.
- Id. See also Cheney FW, Posner KL, Caplan RA. Adverse respiratory events infrequently leading to malpractice suits. A closed claims analysis, Anesthesiol. Vol. 75, No. 6, pp. 932-939 (1991); Peterson GN, Domino KB, et al, Management of the difficult airway: a closed claims analysis, Anesthesiol. Vol. 103, No. 1, pp. 33-39 (2005).
- ASA guidelines 2013, p. 251. In turn, the ASA states that difficult facemask ventilation essentially means that it is not possible for the anesthesiologist to provide adequate air movement in and out of the lungs with a facemask, due to a patient abnormality or an equipment problem; and, difficult tracheal intubation means "multiple attempts" are required to place the breathing tube, either when there is or is not an airway abnormality. Id. at 252.
- Brown CA, Sakles, JC, et al, The Walls Manual of Emergency Airway Management, Ch. 2, Identification of the Difficult and Failed Airway, by Brown CA & Walls RM, p. 36 (Lippincott, Williams & Wilkins 5th ed. 2017).
- Hagberg CA, Hagberg and Benumoff's Airway Management, n2, Ch. 9 by Anderson J, Klock PA, at 185.
- See, e.g., American Sleep Association, Obstructive Sleep Apnea, at: https://www.sleepapnea.org/learn/sleep-apnea/obstructive-sleep-apnea/.
- Brown CA, Sakles, JC, et al, The Walls Manual of Emergency Airway Management, n8, Ch. 3, The Emergency Airway Algorithms, by Brown CA & Walls RM, Fig. 3-3.
- Cass NM, James NR, et al, Difficult direct laryngoscopy complicating intubation for anaesthesia, BMJ Vol. 1, p. 488 (1956); White A, Kander PL, Anatomical factors in difficult direct laryngoscopy, Br. J Anaesth. Vol. 47, p. 468 (1975); Hagberg CA, Handbook of Difficult Airway Management, pp. 18-19 (Churchill Livingston 2000).
- Shiga T, Wajima Z, et al, Predicting difficult intubation in apparently normal patients: A meta-analysis of bedside screening test performance, Anesthesiol. Vol. 103, pp. 429-37 (2005).
- Brown CA, Sakles, JC, et al, The Walls Manual of Emergency Airway Management, n8, Ch. 2.
- Hagberg CA, Hagberg and Benumoff's Airway Management, n2, Ch. 9 by Anderson J, Klock PA, at 190-91.
- Lee A, Fan LT, et al, A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway, Anesth & Analges. Vol. 102, No. 6, pp. 1867-78; Nuckton TJ, Glidden DV, et al, Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea, Sleep Vol. 29, No. 7, pp. 903-08 (Jul. 2006); Hagberg CA, Hagberg and Benumoff's Airway Management, n2, Ch. 9 by Anderson J, Klock PA, at 190.
- For example, a modified Mallampati score of III-IV together with obesity or an abnormally short distance from the chin to the notch of the Adam's apple in a patient (i.e. thyromental distance) results in good accuracy in predicting difficulty in intubation. Hagberg CA, Hagberg and Benumoff's Airway Management, n2, Ch. 9 by Anderson J, Klock PA, at 190 (citing to WH Kim, HJ Ahn, et al, Neck circumference to thyromental distance ratio: a new predictor of difficult intubation in obese patients, Br J Anaesth. Vol. 106, pp. 743-748 (2011)).
- Yentis SM, Lee DJ, Evaluation of an improved scoring system for the grading of direct laryngoscopy, Anaesthes., Vol. 53, No. 11, pp. 1041–44 (1998).
- See, e.g., Hagberg CA, Hagberg and Benumoff's Airway Management, n2, Ch. 8 by Klock PA, at 181-82.
- Id. at 178.
- Id. at 182. See also Loh KS, Irish JC, Traumatic complications of intubation and other airway management procedures, Anesthesiol Clin of N. America Vol. 20, pp. 953-69 (2002); Tachibana N, Niiyama Y, Incidence of cannot intubate-cannot ventilate (CICV): results of a 3-year retrospective multicenter clinical study in a network of university hospitals, J Anesthes. Vol. 29, No. 3, pp. 326-30 (June 2015).
- Brown CA, Sakles, JC, et al, The Walls Manual of Emergency Airway Management, n8, Ch. 2.